Mosquito Vectors (Diptera: Culicidae) and Mosquito-Borne Diseases in North Africa
Abstract
:Simple Summary
Abstract
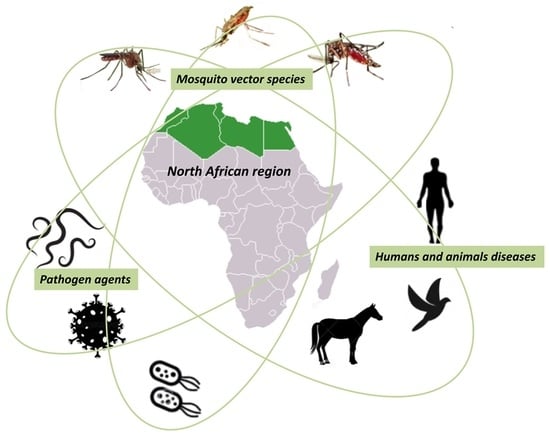
1. Introduction
2. Methodology
3. Salient Data on North Africa
4. Morphology, Life Cycle, Taxonomy, Genomics and Identification Methods of Culicidae
5. Culicidae Fauna of Medical and Veterinary Importance in North Africa
5.1. Sub-Family Culicinae
5.1.1. Aedes (Meigen)
5.1.2. Culex Linnaeus
5.1.3. Culiseta (Felt)
5.2. Sub-Family Anophelinae
Anopheles (Meigen)
6. Mosquito-Borne Diseases in North Africa
6.1. Parasitic Infections
6.1.1. Plasmodium
6.1.2. Filariasis
Wuchereria Bancrofti
Dirofilaria immitis and Dirofilaria repens
6.2. Arboviruses
6.2.1. West Nile Virus (WNV)
6.2.2. Rift Valley Fever (RVF)
6.2.3. Chikungunya Virus (CHIKV)
6.2.4. Dengue
6.2.5. Yellow Fever (YF)
6.2.6. Zika Virus
6.2.7. Sindbis Virus (SINV)
6.2.8. Usutu Virus (USUV)
6.3. Bacteria
7. Mosquito Control Strategies in North Africa
Insecticide Resistance
8. Potential Factors Contributing to the Future Spread of MBDs within the North Africa Region
9. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Weaver, S.C.; Charlier, C.; Vasilakis, N.; Lecuit, M. Zika, Chikungunya, and Other Emerging Vector-Borne Viral Diseases. Annu. Rev. Med. 2017, 69, 395–408. [Google Scholar] [CrossRef] [PubMed]
- Parola, P.; Musso, D.; Raoult, D. Rickettsia felis: The next mosquito-borne outbreak? Lancet Infect. Dis. 2016, 16, 1112–1113. [Google Scholar] [CrossRef] [Green Version]
- World Malaria Report. 2020. Available online: https://www.who.int/teams/global-malaria-programme/reports/world-malaria-report-2020. (accessed on 1 September 2022).
- Tolle, M.A. Mosquito-borne Diseases. Curr. Probl. Pediatr. Adolesc. Health Care 2009, 39, 97–140. [Google Scholar] [CrossRef] [PubMed]
- Ramasamy, R.; Surendran, S.N. Possible impact of rising sea levels on vector-borne infectious diseases. BMC Infect. Dis. 2011, 11, 18. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Blagrove, M.S.C.; Caminade, C.; Waldmann, E.; Sutton, E.R.; Wardeh, M.; Baylis, M. Co-occurrence of viruses and mosquitoes at the vectors’ optimal climate range: An underestimated risk to temperate regions? PLoS Negl. Trop. Dis. 2017, 11, e0005604. [Google Scholar] [CrossRef] [Green Version]
- Semenza, J.C.; Paz, S. Climate change and infectious disease in Europe: Impact, projection and adaptation. Lancet Reg. Health Eur. 2021, 9, 100230. [Google Scholar] [CrossRef]
- Benjelloun, A.; El Harrak, M.; Belkadi, B. West Nile Disease Epidemiology in North-West Africa: Bibliographical Review. Transbound. Emerg. Dis. 2016, 63, e153–e159. [Google Scholar] [CrossRef]
- Tambo, E.; Olalubi, O.A.; Sacko, M. Rift valley fever epidemic in Niger near border with Mali. Lancet Infect. Dis. 2016, 16, 1319–1320. [Google Scholar] [CrossRef]
- Lemine, A.M.M.; Lemrabott, M.A.O.; Ebou, M.H.; Lekweiry, K.M.; Salem, M.S.O.A.; Brahim, K.O.; Moukah, M.O.; Bouraya, I.N.O.; Brengues, C.; Trape, J.-F.; et al. Mosquitoes (Diptera: Culicidae) in Mauritania: A review of their biodiversity, distribution and medical importance. Parasites Vectors 2017, 10, 35. [Google Scholar] [CrossRef] [Green Version]
- Jourdain, F.; Picard, M.; Sulesco, T.; Haddad, N.; Harrat, Z.; Sawalha, S.S.; Günay, F.; Kanani, K.; Shaibi, T.; Akhramenko, D.; et al. Identification of mosquitoes (Diptera: Culicidae): An external quality assessment of medical entomology laboratories in the MediLabSecure Network. Parasites Vectors 2018, 11, 553. [Google Scholar] [CrossRef]
- Jourdain, F.; Samy, A.M.; Hamidi, A.; Bouattour, A.; Alten, B.; Faraj, C.; Roiz, D.; Petrić, D.; Pérez-Ramírez, E.; Velo, E.; et al. Towards harmonisation of entomological surveillance in the Mediterranean area. PLoS Negl. Trop. Dis. 2019, 13, e0007314. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- VectorNet. 2021. Available online: https://www.ecdc.europa.eu/en/about-us/partnerships-and-networks/disease-and-laboratory-networks/vector-net (accessed on 1 September 2022).
- Dedet, J.-P. Edmond and Etienne Sergent. The epic of the Pasteur Institute of Algeria. Rev. Prat. 2012, 62, 1029–1033. [Google Scholar]
- Senevet, G.; Andarelli, L. Les Anophèles de l’Afrique du Nord et du Bassin Méditerranéen; P. Lechevalier: Bois Guillaume, France, 1956. [Google Scholar]
- Senevet, G.; Andarelli, L. Les Moustiques de l’Afrique du Nord et du Bassin Méditerranéen: Les Genres Cu-lex-Uranotaenia-Theobaldia-Orthopodomya et Mansonia; P. Lechevalier: Bois Guillaume, France, 1959. [Google Scholar]
- Brunhes, J.; Rhaim, A.; Geoffroy, B.; Angel, G.; Hervy, J.P. The Mosquitoes of the Mediterranean Africa: An Identification and Training Program; IRD: Montpellier, France, 2000. [Google Scholar]
- Robert, V.; Günay, F.; Le Goff, G.; Boussès, P.; Sulesco, T.; Khalin, A.; Medlock, J.M.; Kampen, H.; Petric, D.; Schaffner, F. Distribution Chart for Euro-Mediterranean Mosquitoes (Western Palaearctic Region). J. Eur. Mosq. Control. Assoc. 2019, 37, 1–28. [Google Scholar]
- Sissani, I.; Boutellis, A.; Ramdan, A.; Hallouane, F.; Chahbar, N.; Bitam, I. Biological effect of the entomopathogenic fungus Metarhi-zium anisopliae variety acridum against the house-mosquito Culex pipiens. Int. J. Bot. Res. 2014, 4, 31–38. [Google Scholar]
- Kharoubi, R.; Rehimi, N.; Khaldi, R.; Haouari-Abderrahim, J.; Soltani, N. Phytochemical Screening and Insecticidal Activities of Essential oil of Mentha × piperita L. (Lamiales: Lamiaceae) and their Enzymatic Properties against Mosquito Culex pipiens L. (Diptera: Culicidae). J. Essent. Oil Bear. Plants 2021, 24, 134–146. [Google Scholar] [CrossRef]
- Merabti, B.; Boumaza, M.; Ouakid, M.; Carvajal, T.M.; Harbach, R.E. An updated checklist of the mosquitoes (Diptera: Culicidae) present in Algeria, with assessments of doubtful records and problematic species. Zootaxa 2021, 5027, 515–545. [Google Scholar] [CrossRef]
- Tahir, D.; Damene, H.; Davoust, B.; Parola, P. First molecular detection of Dirofilaria immitis (Spirurida: Onchocercidae) infection in dogs from Northern Algeria. Comp. Immunol. Microbiol. Infect. Dis. 2017, 51, 66–68. [Google Scholar] [CrossRef]
- Lafri, I.; Prat, C.M.; Bitam, I.; Gravier, P.; Besbaci, M.; Zeroual, F.; Ben-Mahdi, M.H.; Davoust, B.; Leparc-Goffart, I. Seroprevalence of West Nile virus antibodies in equids in the North-East of Algeria and detection of virus circulation in 2014. Comp. Immunol. Microbiol. Infect. Dis. 2017, 50, 8–12. [Google Scholar] [CrossRef]
- Benbetka, S.; Hachid, A.; Benallal, K.; Benbetka, C.; Khaldi, A.; Bitam, I.; Harrat, Z. First field evidence infection of Culex perexiguus by West Nile virus in Sahara Oasis of Algeria. J. Vector Borne Dis. 2018, 55, 305–309. [Google Scholar] [CrossRef]
- Charrel, R.; Berenger, J.-M.; Laroche, M.; Ayhan, N.; Bitam, I.; Delaunay, P.; Parola, P. Neglected vector-borne bacterial diseases and arboviruses in the Mediterranean area. New Microbes New Infect. 2018, 26, S31–S36. [Google Scholar] [CrossRef]
- Lafri, I.; Hachid, A.; Bitam, I. West Nile virus in Algeria: A comprehensive overview. New Microbes New Infect. 2018, 27, 9–13. [Google Scholar] [CrossRef]
- Peel, M.C.; Finlayson, B.L.; McMahon, T.A. Updated world map of the Köppen-Geiger climate classification. Hydrol. Earth Syst. Sci. 2007, 11, 1633–1644. [Google Scholar] [CrossRef] [Green Version]
- Ramsar. Country Profiles. 2017. Available online: https://www.ramsar.org/country-profiles. (accessed on 1 September 2022).
- Hagemeijer, W.; Mundkur, T. Migratory Flyways in Europe, Africa and Asia and the Spread of HPAI H5N1. In Proceedings of the International Scientific Conference on Avian Influenza and Wild Birds, Rome, Italy, 30–31 May 2006. [Google Scholar]
- Arnal, A.; Gómez-Díaz, E.; Cerdà-Cuéllar, M.; Lecollinet, S.; Pearce-Duvet, J.; Busquets, N.; García-Bocanegra, I.; Pagès, N.; Vittecoq, M.; Hammouda, A.; et al. Circulation of a Meaban-Like Virus in Yellow-Legged Gulls and Seabird Ticks in the Western Mediterranean Basin. PLoS ONE 2014, 9, e89601. [Google Scholar] [CrossRef] [PubMed]
- Bouguedour, R.; Ripani, A. Review of the foot and mouth disease situation in North Africa and the risk of introducing the disease into Europe. Rev. Sci. Tech. 2016, 35, 757–768. [Google Scholar] [CrossRef] [PubMed]
- Eurostat. Agriculture Statistics—North Africa and Eastern Mediterranean; Eurostat: Luxembourg, 2017. [Google Scholar]
- Puechmaille, S.J.; Allegrini, B.; Benda, P.; Gürün, K.; Srámek, J.; Ibañez, C.; Juste, J.; Bilgin, R. A new species of the Miniopterus schreibersii species complex (Chiroptera: Miniopteridae) from the Maghreb Region, North Africa. Zootaxa 2014, 3794, 108–124. [Google Scholar] [CrossRef] [PubMed]
- Khelfaoui, F.; Kebaci, A.; Benyacoub, S. New Data on Insecta and Acarina Parasitizing Bats (Mammalia: Chiroptera) in Numidia, Eastern Algeria. Bull. Soc. Zool. Fr. 2018, 143, 63–73. [Google Scholar]
- Becker, N.; Petric, D.; Zgomba, M.; Boase, C.; Dahl, C.; Madon, M.; Kaiser, A. Mosquitoes and Their Control; Springer Science & Business Media: Berlin/Heidelberg, Germany, 2010. [Google Scholar]
- EPA. CDC. Joint Statement on Mosquito Control in the United States. 2012. Available online: https://www.epa.gov/mosquitocontrol/joint-statement-mosquito-control-united-states#:~:text=Mosquito%20control%20activities%20are%20important,when%20requested%20by%20the%20states (accessed on 1 September 2022).
- Wilkerson, R.C.; Linton, Y.-M.; Fonseca, D.; Schultz, T.R.; Price, D.C.; Strickman, D.A. Making Mosquito Taxonomy Useful: A Stable Classification of Tribe Aedini that Balances Utility with Current Knowledge of Evolutionary Relationships. PLoS ONE 2015, 10, e0133602. [Google Scholar] [CrossRef]
- Reinert, J.F. List of abbreviations for currently valid generic-level taxa in family Culicidae (Diptera). Eur. Mosq. Bull. 2009, 27, 68–76. [Google Scholar]
- Motta, D.; Santos, A.B.; Winkler, I.; Machado, B.A.S.; Pereira, D.A.D.I.; Cavalcanti, A.M.; Fonseca, E.O.L.; Kirchner, F.; Badaró, R. Application of convolutional neural networks for classification of adult mosquitoes in the field. PLoS ONE 2019, 14, e0210829. [Google Scholar] [CrossRef] [Green Version]
- Schaffner, F. Identifying a mosquito: Traditional morphology and new molecular techniques associated for integrated taxonomy. Rev. Francoph. Lab. 2020, 524, 24–33. [Google Scholar]
- Zamyatin, A.; Avdeyev, P.; Liang, J.; Sharma, A.; Chen, C.; Lukyanchikova, V.; Alexeev, N.; Tu, Z.; Alekseyev, M.A.; Sharakhov, I.V. Chromosome-level genome assemblies of the malaria vectors Anopheles coluzzii and Anopheles arabiensis. GigaScience 2021, 10, giab017. [Google Scholar] [CrossRef] [PubMed]
- Jiang, X.; Peery, A.; Hall, A.B.; Sharma, A.; Chen, X.-G.; Waterhouse, R.M.; Komissarov, A.; Riehle, M.M.; Shouche, Y.; Sharakhova, M.V.; et al. Genome analysis of a major urban malaria vector mosquito, Anopheles stephensi. Genome Biol. 2014, 15, 459. [Google Scholar] [CrossRef] [PubMed]
- Chen, X.-G.; Jiang, X.; Gu, J.; Xu, M.; Wu, Y.; Deng, Y.; Zhang, C.; Bonizzoni, M.; Dermauw, W.; Vontas, J.; et al. Genome sequence of the Asian Tiger mosquito, Aedes albopictus, reveals insights into its biology, genetics, and evolution. Proc. Natl. Acad. Sci. USA 2015, 112, E5907–E5915. [Google Scholar] [CrossRef] [Green Version]
- Nene, V.; Wortman, J.R.; Lawson, D.; Haas, B.; Kodira, C.; Tu, Z.; Loftus, B.; ** using protein signatures from larval and pupal exuviae. Parasites Vectors 2020, 13, 161. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sevestre, J.; Diarra, A.Z.; Laroche, M.; Almeras, L.; Parola, P. Matrix-assisted laser desorption/ionization time-of-flight mass spectrometry: An emerging tool for studying the vectors of human infectious diseases. Future Microbiol. 2021, 16, 323–340. [Google Scholar] [CrossRef] [PubMed]
- Abdellahoum, Z.; Nebbak, A.; Lafri, I.; Kaced, A.; Bouhenna, M.M.; Bachari, K.; Boumegoura, A.; Agred, R.; Boudchicha, R.H.; Smadi, M.A.; et al. Identification of Algerian field-caught mosquito vectors by MALDI-TOF MS. Vet. Parasitol. Reg. Stud. Rep. 2022, 31, 100735. [Google Scholar] [CrossRef]
- Izri, A.; Bitam, I.; Charrel, R.N. First entomological documentation of Aedes (Stegomyia) albopictus (Skuse, 1894) in Algeria. Clin. Microbiol. Infect. 2011, 17, 1116–1118. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Benallal, K.; Allal-Ikhlef, A.; Benhamouda, K.; Schaffner, F.; Harrat, Z. First report of Aedes (Stegomyia) albopictus (Diptera: Culicidae) in Oran, West of Algeria. Acta Trop. 2016, 164, 411–413. [Google Scholar] [CrossRef] [PubMed]
- Shoukry, N.M.; Elwan, M.A.; Morsy, T.A. Aedes Aegypti (Linnaeus) Re-Emerging in Southern Egypt. J. Egypt. Soc. Parasitol. 2012, 42, 41–50. [Google Scholar] [CrossRef]
- Bèji, M.; Rhim, A.; Roiz, D.; Bouattour, A. Ecophysiological characterization and molecular differentiation of Culex pipiens forms (Diptera: Culicidae) in Tunisia. Parasites Vectors 2017, 10, 327. [Google Scholar] [CrossRef] [Green Version]
- Mikhail, M.W.; Al-Bursheed, K.M.; El-Halim, A.S.A.; Morsy, T.A. Studies on mosquito borne dieases in Egypt and Qatar. J. Egypt. Soc. Parasitol. 2009, 39, 745–756. [Google Scholar]
- Amara Korba, R.; Boukraa, S.; Alayat, M.S.; Bendjeddou, M.L.; Francis, F.; Boubidi, S.C.; Bouslama, Z. Preliminary report of mosquitoes survey at Tonga Lake (North-East Algeria). Adv. Environ. Biol. 2015, 9, 288–294. [Google Scholar]
- Trari, B.; Dakki, M.; Harbach, R.E. An updated checklist of the Culicidae (Diptera) of Morocco, with notes on species of historical and current medical importance. J. Vector Ecol. 2017, 42, 94–104. [Google Scholar] [CrossRef] [Green Version]
- Dyab, A.K.; Galal, L.; Mahmoud, A.E.-S.; Mokhtar, Y. Xenomonitoring of Different Filarial Nematodes Using Single and Multiplex PCR in Mosquitoes from Assiut Governorate, Egypt. Korean J. Parasitol. 2015, 53, 77–83. [Google Scholar] [CrossRef] [PubMed]
- Shaikevich, E.V.; Vinogradova, E.B.; Bouattour, A.; de Almeida, A.P.G. Genetic diversity of Culex pipiens mosquitoes in distinct populations from Europe: Contribution of Cx. quinquefasciatus in Mediterranean populations. Parasites Vectors 2016, 9, 47. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Berčič, R.L.; Bányai, K.; Růžek, D.; Fehér, E.; Domán, M.; Danielová, V.; Bakonyi, T.; Nowotny, N. Phylogenetic Analysis of Lednice Orthobunyavirus. Microorganisms 2019, 7, 447. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tabbabi, A.; Simard, F.; Brengues, C.; Rhim, A.; Boussès, P.; Bouratbine, A.; Fontenille, D.; Ben-Alaya-Bouafif, N.; Daaboub, J.; Aoun, K. Larval Habitats Characterization and Species Composition of Anopheles Mosquitoes in Tunisia, with Particular Attention to Anopheles maculipennis Complex. Am. J. Trop. Med. Hyg. 2015, 92, 653–659. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Duvallet, G.; Fontenille, D.; Robert, V. Entomologie Médicale et Vétérinaire; Editions Quae: Versailles, France, 2017. [Google Scholar]
- Faraj, C.; Adlaoui, E.; Rhajaoui, M.; Lyagoubi, M. Estimation of malaria transmission in high-risk provinces of Morocco. East. Mediterr. Health J. 2003, 9, 542–547. [Google Scholar] [CrossRef]
- Hamaidia, H.; Berchi, S. Biosystematic study of culicidae (Diptera, Nematocera) nuisance source in Tébessa (Algeria). J. Entomol. Zool. Stud. 2018, 6, 1226–1231. [Google Scholar]
- Boudemagh, N.; Bendali-Saoudi, F.; Soltani, N. Inventory of Culicidae (Diptera: Nematocera) in the region of Collo (North-East Algeria). Ann. Biol. Res. 2013, 4, 94–99. [Google Scholar]
- Boubidi, S.C.; Gassen, I.; Khechache, Y.; Lamali, K.; Tchicha, B.; Brengues, C.; Menegon, M.; Severini, C.; Fontenille, D.; Harrat, Z. PlasmodiumfalciparumMalaria, Southern Algeria, 2007. Emerg. Infect. Dis. 2010, 16, 301–303. [Google Scholar] [CrossRef]
- El-Bahnasawy, M.M.; Fadil, E.E.; Morsy, T.A. Mosquito vectors of infectious diseases: Are they neglected health disaster in Egypt? J. Egypt Soc. Parasitol. 2013, 43, 373–386. [Google Scholar]
- Frank, J.H.; Service, M.W. Medical Entomology for Students. Fla. Èntomol. 2000, 83, 384. [Google Scholar] [CrossRef]
- Bonizzoni, M.; Gasperi, G.; Chen, X.; James, A.A. The invasive mosquito species Aedes albopictus: Current knowledge and future perspectives. Trends Parasitol. 2013, 29, 460–468. [Google Scholar] [CrossRef]
- Lafri, I.; Bitam, I.; Beneldjouzi, A.; Ben Mahdi, M.H. An inventory of mosquitoes (Diptera: Culicidae) in Algeria. Bull. Soc. Zool. Fr. 2014, 139, 255–261. [Google Scholar]
- Bennouna, A.; Balenghien, T.; EL Rhaffouli, H.; Schaffner, F.; Garros, C.; Gardès, L.; Lhor, Y.; Hammoumi, S.; Chlyeh, G.; Fihri, O.F. First record of Stegomyia albopicta (=Aedes albopictus) in Morocco: A major threat to public health in North Africa? Med. Vet. Èntomol. 2016, 31, 102–106. [Google Scholar] [CrossRef] [PubMed]
- Amraoui, F.; Ben Ayed, W.; Madec, Y.; Faraj, C.; Himmi, O.; Btissam, A.; Sarih, M.; Failloux, A.-B. Potential of Aedes albopictus to cause the emergence of arboviruses in Morocco. PLoS Negl. Trop. Dis. 2019, 13, e0006997. [Google Scholar] [CrossRef] [Green Version]
- Failloux, A.-B.; Bouattour, A.; Faraj, C.; Gunay, F.; Haddad, N.; Harrat, Z.; Jancheska, E.; Kanani, K.; Kenawy, M.A.; Kota, M.; et al. Surveillance of Arthropod-Borne Viruses and Their Vectors in the Mediterranean and Black Sea Regions Within the MediLabSecure Network. Curr. Trop. Med. Rep. 2017, 4, 27–39. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Benallal, K.E.; Garni, R.; Bouiba, L.; Harrat, Z. First Detection of Aedes (Stegomyia) albopictus (Diptera: Culicidae) in Algiers, the Capital City of Algeria. J. Arthropod-Borne Dis. 2019, 13, 420. [Google Scholar] [CrossRef] [PubMed]
- Arroussi, D.E.R.; Bouaziz, A.; Boudjelida, H. Mosquito survey reveals the first record of Aedes (Diptera: Culicidae) species in urban area, Annaba district, Northeastern Algeria. Pol. J. Èntomol. 2021, 90, 14–26. [Google Scholar] [CrossRef]
- Bouattour, A.; Khrouf, F.; Rhim, A.; M’Ghirbi, Y. First Detection of the Asian Tiger Mosquito, Aedes (Stegomyia) albopictus (Diptera: Culicidae), in Tunisia. J. Med. Èntomol. 2019, 56, 1112–1115. [Google Scholar] [CrossRef] [PubMed]
- Kamal, M.; Kenawy, M.A.; Rady, M.H.; Khaled, A.S.; Samy, A.M. Map** the global potential distributions of two arboviral vectors Aedes aegypti and Ae. albopictus under changing climate. PLoS ONE 2018, 13, e0210122. [Google Scholar] [CrossRef] [Green Version]
- Brustolin, M.; Talavera, S.; Nuñez, A.; Santamaría, C.; Rivas, R.; Pujol, N.; Valle, M.; Verdún, M.; Brun, A.; Pagès, N.; et al. Rift Valley fever virus and European mosquitoes: Vector competence of Culex pipiens and Stegomyia albopicta (=Aedes albopictus). Med. Vet. Èntomol. 2017, 31, 365–372. [Google Scholar] [CrossRef] [Green Version]
- Paupy, C.; Delatte, H.; Bagny, L.; Corbel, V.; Fontenille, D. Aedes albopictus, an arbovirus vector: From the darkness to the light. Microbes Infect. 2009, 11, 1177–1185. [Google Scholar] [CrossRef] [PubMed]
- Cancrini, G.; Scaramozzino, P.; Gabrielli, S.; Di Paolo, M.; Toma, L.; Romi, R. Aedes albopictus and Culex pipiens Implicated as Natural Vectors of Dirofilaria repens in Central Italy. J. Med. Èntomol. 2007, 44, 1064–1066. [Google Scholar] [CrossRef]
- Socolovschi, C.; Pagés, F.; Raoult, D. Rickettsia felis in Aedes albopictus Mosquitoes, Libreville, Gabon. Emerg. Infect. Dis. 2012, 18, 1687–1689. [Google Scholar] [CrossRef] [PubMed]
- Lounibos, L.P.; Kramer, L.D. Invasiveness of Aedes aegypti and Aedes albopictus and Vectorial Capacity for Chikungunya Virus. J. Infect. Dis. 2016, 214, S453–S458. [Google Scholar] [CrossRef] [Green Version]
- Heikal, O.M.; El-Bahnasawy, M.M.; Morsy, A.T.; Khalil, H.H. Aedes aegypti re-emerging in Egypt: A review and what should be done? J. Egypt. Soc. Parasitol. 2011, 41, 801–814. [Google Scholar]
- Arsevska, E.; Hellal, J.; Mejri, S.; Hammami, S.; Marianneau, P.; Calavas, D.; Hénaux, V. Identifying Areas Suitable for the Occurrence of Rift Valley Fever in North Africa: Implications for Surveillance. Transbound. Emerg. Dis. 2015, 63, 658–674. [Google Scholar] [CrossRef]
- Mancini, G.; Montarsi, F.; Calzolari, M.; Capelli, G.; Dottori, M.; Ravagnan, S.; Lelli, D.; Chiari, M.; Santilli, A.; Quaglia, M.; et al. Mosquito species involved in the circulation of West Nile and Usutu viruses in Italy. Vet. Ital. 2017, 53, 97–110. [Google Scholar] [CrossRef]
- Ben Ayed, W.; Amraoui, F.; M’Ghirbi, Y.; Schaffner, F.; Rhaim, A.; Failloux, A.-B.; Bouattour, A. A Survey of Aedes (Diptera: Culicidae) Mosquitoes in Tunisia and the Potential Role of Aedes detritus and Aedes caspius in the Transmission of Zika Virus. J. Med. Èntomol. 2019, 56, 1377–1383. [Google Scholar] [CrossRef]
- Mackenzie-Impoinvil, L.; Impoinvil, D.E.; Galbraith, S.E.; Dillon, R.J.; Ranson, H.; Johnson, N.; Fooks, A.R.; Solomon, T.; Baylis, M. Evaluation of a temperate climate mosquito, Ochlerotatus detritus (=Aedes detritus), as a potential vector of Japanese encephalitis virus. Med. Vet. Èntomol. 2014, 29, 1–9. [Google Scholar] [CrossRef]
- Blagrove, M.S.C.; Sherlock, K.; Chapman, G.E.; Impoinvil, D.E.; McCall, P.J.; Medlock, J.M.; Lycett, G.; Solomon, T.; Baylis, M. Evaluation of the vector competence of a native UK mosquito Ochlerotatus detritus (Aedes detritus) for dengue, chikungunya and West Nile viruses. Parasites Vectors 2016, 9, 452. [Google Scholar] [CrossRef] [Green Version]
- Moutailler, S.; Krida, G.; Schaffner, F.; Vazeille, M.; Failloux, A.-B. Potential Vectors of Rift Valley Fever Virus in the Mediterranean Region. Vector-Borne Zoonotic Dis. 2008, 8, 749–754. [Google Scholar] [CrossRef] [PubMed]
- O’Donnell, K.L.; Bixby, M.A.; Morin, K.J.; Bradley, D.S.; Vaughan, J.A. Potential of a Northern Population of Aedes vexans (Diptera: Culicidae) to Transmit Zika Virus. J. Med. Èntomol. 2017, 54, 1354–1359. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kurucz, K.; Kepner, A.; Krtinic, B.; Zana, B.; Földes, F.; Bányai, K.; Oldal, M.; Jakab, F.; Kemenesi, G. First molecular identification of Dirofilaria spp. (Onchocercidae) in mosquitoes from Serbia. Parasitol. Res. 2016, 115, 3257–3260. [Google Scholar] [CrossRef] [PubMed]
- Anderson, J.F.; Main, A.J.; Ferrandino, F.J. Horizontal and Vertical Transmission of West Nile Virus by Aedes vexans (Diptera: Culicidae). J. Med. Èntomol. 2020, 57, 1614–1618. [Google Scholar] [CrossRef]
- Farajollahi, A.; Fonseca, D.M.; Kramer, L.D.; Kilpatrick, A.M. “Bird biting” mosquitoes and human disease: A review of the role of Culex pipiens complex mosquitoes in epidemiology. Infect. Genet. Evol. 2011, 11, 1577–1585. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Amraoui, F.; Tijane, M.; Sarih, M.; Failloux, A.-B. Molecular evidence of Culex pipiens form molestus and hybrids pipiens/molestus in Morocco, North Africa. Parasites Vectors 2012, 5, 83. [Google Scholar] [CrossRef] [Green Version]
- Benallal, K.; Benbetka, S.; Tail, G.; Harrat, Z. Molecular characterization of Culex pipiens (Diptera, Culicidae) in Reghaïa lake, Algeria. Ann. Biol. Sci. 2015, 3, 20–24. [Google Scholar]
- Korba, R.A.; Alayat, M.S.; Bouiba, L.; Boudrissa, A.; Bouslama, Z.; Boukraa, S.; Francis, F.; Failloux, A.-B.; Boubidi, S.C. Ecological differentiation of members of the Culex pipiens complex, potential vectors of West Nile virus and Rift Valley fever virus in Algeria. Parasites Vectors 2016, 9, 455. [Google Scholar] [CrossRef] [Green Version]
- Amraoui, F.; Krida, G.; Bouattour, A.; Rhim, A.; Daaboub, J.; Harrat, Z.; Boubidi, S.-C.; Tijane, M.; Sarih, M.; Failloux, A.-B. Culex pipiens, an Experimental Efficient Vector of West Nile and Rift Valley Fever Viruses in the Maghreb Region. PLoS ONE 2012, 7, e36757. [Google Scholar] [CrossRef] [Green Version]
- Khalifa, R.M.; El-Nadi, N.A.; Ahmed, A.M.; Hassan, F.A. Histological and PCR xenomonitoring of culicine mosquitoes for filarial infestation in Sohag Governorate, upper Egypt. J. Egypt Soc. Parasitol. 2013, 43, 591–600. [Google Scholar]
- Samy, A.; Elaagip, A.H.; Kenawy, M.; Ayres, C.F.J.; Peterson, A.T.; Soliman, D. Climate Change Influences on the Global Potential Distribution of the Mosquito Culex quinquefasciatus, Vector of West Nile Virus and Lymphatic Filariasis. PLoS ONE 2016, 11, e0163863. [Google Scholar] [CrossRef]
- Guedes, D.R.; Paiva, M.H.; Donato, M.M.; Barbosa, P.P.; Krokovsky, L.; Rocha, S.W.D.S.; LA Saraiva, K.; Crespo, M.M.; Rezende, T.M.; Wallau, G.L.; et al. Zika virus replication in the mosquito Culex quinquefasciatus in Brazil. Emerg. Microbes Infect. 2017, 6, 1–11. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hanafi, H.A.; Fryauff, D.J.; Saad, M.D.; Soliman, A.K.; Mohareb, E.W.; Medhat, I.; Zayed, A.B.; Szumlas, D.E.; Earhart, K.C. Virus isolations and high population density implicate Culex antennatus (Becker) (Diptera: Culicidae) as a vector of Rift Valley Fever virus during an outbreak in the Nile Delta of Egypt. Acta Trop. 2011, 119, 119–124. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ratovonjato, J.; Olive, M.-M.; Tantely, L.M.; Andrianaivolambo, L.; Tata, E.; Razainirina, J.; Jeanmaire, E.; Reynes, J.-M.; Elissa, N. Detection, Isolation, and Genetic Characterization of Rift Valley Fever Virus from Anopheles (Anopheles) coustani, Anopheles (Anopheles) squamosus, and Culex (Culex) antennatus of the Haute Matsiatra Region, Madagascar. Vector-Borne Zoonotic Dis. 2011, 11, 753–759. [Google Scholar] [CrossRef] [PubMed]
- Kolodziejek, J.; Pachler, K.; Bin, H.; Mendelson, E.; Shulman, L.M.; Orshan, L.; Nowotny, N. Barkedji virus, a novel mosquito-borne flavivirus identified in Culex perexiguus mosquitoes, Israel, 2011. J. Gen. Virol. 2013, 94, 2449–2457. [Google Scholar] [CrossRef]
- McIntosh, B.M.; Jupp, P.G.; Dos Santos, I.; Meenehan, G.M. Epidemics of West Nile and Sindbis viruses in South Africa with Culex (Culex) univittatus Theobald as vector. S. Afr. J. Sci. 1976, 72, 295–300. [Google Scholar]
- Miller, B.R.; Nasci, R.S.; Lutwama, J.; Godsey, M.S.; Savage, H.; Lanciotti, R.; Peters, C.J. First field evidence for natural vertical transmission of West Nile virus in Culex univittatus complex mosquitoes from Rift Valley province, Kenya. Am. J. Trop. Med. Hyg. 2000, 62, 240–246. [Google Scholar] [CrossRef] [Green Version]
- Ergünay, K.; Litzba, N.; Brinkmann, A.; Gunay, F.; Kar, S.; Öter, K.; Örsten, S.; Sarıkaya, Y.; Alten, B.; Nitsche, A.; et al. Isolation and genomic characterization of Culex theileri flaviviruses in field-collected mosquitoes from Turkey. Infect. Genet. Evol. 2016, 46, 138–147. [Google Scholar] [CrossRef] [Green Version]
- Carnevale, P.; Robert, V. Les Anophèles Biologie, Transmission du Plasmodium et Lutte Antivectorielle; IRD: Montpellier, France, 2009. [Google Scholar]
- Larhbali, Y.; Belghyti, D.; El Guamri, Y.; Lahlou, O.; El Kharrim, K.; Kirami, A.; Khamri, Z. Epidemiology of imported malaria and entomological study of breeding sites of potential risk areas in the province of Khemisset (Morocco). Med. Sante Trop. 2014, 24, 397–402. [Google Scholar] [CrossRef]
- Laboudi, M.; Faraj, C.; Sadak, A.; Harrat, Z.; Boubidi, S.C.; Harbach, R.E.; EL Aouad, R.; Linton, Y.-M. DNA barcodes confirm the presence of a single member of the Anopheles maculipennis group in Morocco and Algeria: An. sicaulti is conspecific with An. labranchiae. Acta Trop. 2011, 118, 6–13. [Google Scholar] [CrossRef]
- Mahmoud, D.M.; Hussein, H.M.; El Gozamy, B.M.R.; Thabet, H.S.; Hassan, M.A.; Meselhey, R.A.-A. Screening of Plasmodium parasite in vectors and humans in three villages in Aswan Governorate, Egypt. J. Parasit. Dis. 2018, 43, 158–163. [Google Scholar] [CrossRef]
- Faraj, C.; Adlaoui, E.; Ouahabi, S.; Rhajaoui, M.; Fontenille, D.; Lyagoubi, M. Entomological investigations in the region of the last malaria focus in Morocco. Acta Trop. 2009, 109, 70–73. [Google Scholar] [CrossRef] [PubMed]
- Smith, D.M. Mosquito records from the Republic of Niger, with reference to the construction of the new ‘Trans-Sahara Highway’. J. Trop. Med. Hyg. 1981, 84, 95–100. [Google Scholar] [PubMed]
- Yamany, A.S.; Adham, F.K.; Mehlhorn, H. Structural changes of the follicular cells during developmental stages of the malaria vector mosquitoes Anopheles pharoensis (Diptera: Culicidae) in Egypt. Parasitol. Res. 2014, 113, 4233–4241. [Google Scholar] [CrossRef] [PubMed]
- Wassim, N.M. Secondray Structure and Sequenceofits2-Rdna of the Egyptian Malaria Vectoranopheles Pharoensis (Theobald). J. Egypt. Soc. Parasitol. 2014, 44, 197–204. [Google Scholar] [CrossRef]
- Epelboin, Y.; Talaga, S.; Epelboin, L.; Dusfour, I. Zika virus: An updated review of competent or naturally infected mosquitoes. PLoS Negl. Trop. Dis. 2017, 11, e0005933. [Google Scholar] [CrossRef] [PubMed]
- Tchicha, B. Historique de la Lutte Antipaludique en Algérie. Service du Paludisme et des Maladies Parasitaires; INSP: Indian Land, SC, USA, 2011. [Google Scholar]
- Hammadi, D.; Boubidi, S.C.; Chaib, S.E.; Saber, A.; Khechache, Y.; Gasmi, M.; Harrat, Z. Malaria in Algerian Sahara. Bull. Soc. Pathol. Exot. 2009, 102, 185–192. [Google Scholar]
- Gebreel, A.O.; Gilles, H.M.; Prescott, J.E. Studies on the sero-epidemiology of endemic diseases in Libya, IV Malaria. Ann. Trop. Med. Parasitol. 1985, 79, 341–347. [Google Scholar] [CrossRef]
- Trari, B.; Carnevale, P. Malaria in Morocco: From pre-elimination to elimination, what risks for the future? Bull. Soc. Pathol. Exot. 2011, 104, 291–295. [Google Scholar] [CrossRef]
- Mesbah, S. Maladies infectieuses émergentes et réémergentes: Le risque et la riposte en Algérie. Med. Trop. 2009, 69, 27–32. [Google Scholar]
- Lalami, A.E.O.; Cherigui, M.; Koraichi, S.I.; Maniar, S.; El Maimouni, N.; Rhajaoui, M. Imported malaria in northern central Morocco, 1997–2007. Sante 2009, 19, 43–47. [Google Scholar] [CrossRef]
- Kandeel, A.; Haggag, A.; El Fetouh, M.A.; Refaey, S.; Naiel, M.; Hassan, A.; Ramzy, R. Control of malaria outbreak due to Plasmodium vivax in Aswan Governorate, Egypt. East. Mediterr. Health J. 2016, 22, 274–279. [Google Scholar] [CrossRef] [PubMed]
- Martelli, G.; Girometti, N.; Vanino, E.; Bottieau, E.; Viale, P. Plasmodium falciparum malaria in migrants who transited Libya—Where did they contract malaria? Travel Med. Infect. Dis. 2015, 13, 499–500. [Google Scholar] [CrossRef]
- WHO. World Health Organization: Algeria and Argentina Certified Malaria-Free by WHO; WHO: Geneva, Switzerland, 2019. [Google Scholar]
- Mendis, K. Eliminating malaria should not be the end of vigilance. Nature 2019, 573, 7. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hotez, P.J.; Savioli, L.; Fenwick, A. Neglected Tropical Diseases of the Middle East and North Africa: Review of Their Prevalence, Distribution, and Opportunities for Control. PLoS Negl. Trop. Dis. 2012, 6, e1475. [Google Scholar] [CrossRef] [Green Version]
- Abdel-Shafi, I.R.; Shoeib, E.Y.; Attia, S.S.; Rubio, J.M.; Edmardash, Y.; El-Badry, A.A. Mosquito identification and molecular xenomon-itoring of lymphatic filariasis in selected endemic areas in giza and qualioubiya governorates. Egypt. J. Egypt Soc. Parasitol. 2016, 46, 93–100. [Google Scholar]
- Abdel-Shafi, I.R.; Shoieb, E.Y.; Attia, S.S.; Rubio, J.M.; Ta-Tang, T.-H.; El-Badry, A.A. Molecular identification and phylogenetic analysis of Wuchereria bancrofti from human blood samples in Egypt. Parasitol Res. 2017, 116, 963–970. [Google Scholar] [CrossRef]
- Mehdi, B. Prevalence of canine Dirofilaria immitis infection in the city of Algiers, Algeria. Afr. J. Agric. Res. 2009, 4, 1097–1100. [Google Scholar]
- Khatat, S.E.; Khallaayoune, K.; Errafyk, N.; van Gool, F.; Duchateau, L.; Daminet, S.; Kachani, M.; El Amri, H.; Azrib, R.; Sahibi, H. Detection of Anaplasma spp. and Ehrlichia spp. anibodies, and Dirofilaria immitis antigens in dogs from seven locations of Morocco. Vet. Parasitol. 2017, 239, 86–89. [Google Scholar] [CrossRef] [PubMed]
- Rjeibi, M.R.; Rouatbi, M.; Mabrouk, M.; Tabib, I.; Rekik, M.; Gharbi, M. Molecular Study of Dirofilaria immitis and Dirofilaria repens in Dogs from Tunisia. Transbound. Emerg. Dis. 2016, 64, 1505–1509. [Google Scholar] [CrossRef]
- Dyab, A.K.; Galal, L.A.; Mahmoud, A.E.; Mokhtar, Y. Finding Wolbachia in Filarial larvae and Culicidae Mosquitoes in Upper Egypt Governorate. Korean J. Parasitol. 2016, 54, 265–272. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Soussi, A.; Farah, K.F.; Zermani, R.; Rammeh, S.; Ismail, O.; Zakraoui, A.; Atallah, K.; Ben, J.S. Subcutaneous dirofilariasis due to Diro-filaria repens in Tunisia: A case involving the scrotum. Med. Trop. 2004, 64, 375–378. [Google Scholar]
- Makni, F.; Hachicha, L.; Abdelkafi, N.; Guiaa, N.; Sellami, H.; Sellami, T.; Ayadi, A. Subcutaneous Dirofilaria repens dirofilariasis in the Sfax region (Tunisia). Ann. Dermatol. Venereol. 2007, 134, 53–54. [Google Scholar] [CrossRef]
- Kaouech, E.; Becheur, M.; Cheikh, M.; Belhadj, S.; Kallel, K.; Chaker, E. Subcutaneous dirofilariasis of the upper lip in Tunisia. Sante 2010, 20, 47–48. [Google Scholar]
- Ziadi, S.; Trimeche, M.; Mestiri, S.; Mokni, M.; Trabelsi, A.; Ben, A.A.; Ben, S.M.; Ben Hadj, H.F.; Korbi, S. Human subconjunctival diro-filariasis: Two Tunisian case studies. J. Fr. Ophtalmol. 2005, 28, 773.e1–773.e4. [Google Scholar] [CrossRef]
- Sassi, S.H.; Abid, L.; Dhouib, R.; Mrad, K.; Bouguila, H.; Abbes, I.; Driss, M.; Ben, G.R.; Ben, R.K. Conjunctival dirofilariasis due to Diro-filaria Repens. A new Tunisian case. J. Fr. Ophtalmol. 2006, 29, e5. [Google Scholar]
- Saïed, W.; Amara, K.; Bouchoucha, S.; Khaled, S.; Mrad, K.; Nessib, M.; Smida, M.; Ben Ghachem, M. An unusual cause of hand nodule: Peri-tendon dirofilariasis. Chir. Main. 2011, 30, 66–68. [Google Scholar] [CrossRef]
- Ben Hassouna, J.; Jbir, I.; Mezghani, B.; El Amine, O.; Zemni, I.; Mrad, K.; Ben Dhieb, T.; Gamoudi, A.; Rahal, K. Dirofilariasis of the breast: Two new cases in Tunisia. Med. Sante. Trop. 2015, 25, 327–330. [Google Scholar] [CrossRef]
- Al-Kappany, Y.M.; Lappin, M.R.; Kwok, O.C.H.; Abu-Elwafa, S.A.; Hilali, M.A.; Dubey, J.P. Seroprevalence of Toxoplasma gondii and Concurrent Bartonella spp., Feline Immunodeficiency Virus, Feline Leukemia Virus, and Dirofilaria immitis Infections in Egyptian Cats. J. Parasitol. 2011, 97, 256–258. [Google Scholar] [CrossRef]
- Abdel-Rahman, S.M.; Mahmoud, A.E.; Galal, L.A.A.; Gustinelli, A.; Pampiglione, S. Three new cases of human infection with Dirofilaria repens, one pulmonary and two subcutaneous, in the Egyptian governorate of Assiut. Ann. Trop. Med. Parasitol. 2008, 102, 499–507. [Google Scholar] [CrossRef]
- Mayer, S.V.; Tesh, R.B.; Vasilakis, N. The emergence of arthropod-borne viral diseases: A global prospective on dengue, chikungunya and zika fevers. Acta Trop. 2016, 166, 155–163. [Google Scholar] [CrossRef] [PubMed]
- Metallaoui, A. Renforcement de la Surveillance et des Systèmes D’alerte Pour la Fièvre Catarrhale Ovine, la Fièvre du Nil Occi-Dentale et la Rage au Maroc, Algérie et Tunisie. 2008. Available online: https://www.ipcinfo.org/fileadmin/user_upload/faoectad/library/WN%20Algerie.pdf (accessed on 1 September 2022).
- El-Harrak, M.; Le Guenno, B.; Gounon, P. Isolation of West Nile Virus in Morocco. Virologie 1997, 1, 248–249. [Google Scholar]
- Le Guenno, B.; Bougermouh, A.; Azzam, T.; Bouakaz, R. West Nile: A deadly Virus? Lancet 1996, 348, 1315. [Google Scholar] [CrossRef]
- Giese, C.; Ait El Belghiti, F.; Barboza, P. National EpiSouth Focal Points. West Nile Virus Circulation in the Episouth Countries and Neighbouring Areas Seasons 2010 and 2011 Update 1st July 2012. 2012. Available online: http://www.episouthnetwork.org/sites/default/files/bulletin_file/note_west_nile_episouth_2010_2011_july2012.pdf. (accessed on 1 September 2022).
- Institut de Veille Sanitaire. Bulletin Hebdomadaire International N°369: 10 au 16 Octobre 2012; Institut de Veille Sanitaire: Paris, France, 2012. [Google Scholar]
- Ben Hassine, T.; de Massis, F.; Calistri, P.; Savini, G.; Mohamed, B.B.; Ranen, A.; Di Gennaro, A.; Sghaier, S.; Hammami, S. First Detection of Co-circulation of West Nile and Usutu Viruses in Equids in the South-west of Tunisia. Transbound. Emerg. Dis. 2014, 61, 385–389. [Google Scholar] [CrossRef]
- Wasfi, F.; Dachraoui, K.; Cherni, S.; Bosworth, A.; Barhoumi, W.; Dowall, S.; Chelbi, I.; Derbali, M.; Zoghlami, Z.; Beier, J.; et al. West Nile virus in Tunisia, 2014: First isolation from mosquitoes. Acta Trop. 2016, 159, 106–110. [Google Scholar] [CrossRef]
- Shaibi, T.; Saadawi, W.K.; Aghila, H.; Annajar, B.B. Prevalence of IgG antibodies for the West Nile virus in human population in Tripoli, Libya. J. Vector Borne Dis. 2017, 54, 183–186. [Google Scholar]
- Hachid, A.; Beloufa, M.; Seghier, M.; Bahoura, N.; Dia, M.; Fall, G.; Sall, A. Evidence of West Nile virus circulation among humans in central northern Algeria. New Microbes New Infect. 2019, 29, 100512. [Google Scholar] [CrossRef]
- Conte, A.; Candeloro, L.; Ippoliti, C.; Monaco, F.; de Massis, F.; Bruno, R.; Di Sabatino, D.; Danzetta, M.L.; Benjelloun, A.; Belkadi, B.; et al. Spatio-Temporal Identification of Areas Suitable for West Nile Disease in the Mediterranean Basin and Central Europe. PLoS ONE 2015, 10, e0146024. [Google Scholar] [CrossRef]
- Saiz, J.-C. Animal and Human Vaccines against West Nile Virus. Pathogens 2020, 9, 1073. [Google Scholar] [CrossRef]
- Kaiser, J.A.; Wang, T.; Barrett, A.D. Virulence determinants of West Nile virus: How can these be used for vaccine design? Futur. Virol. 2017, 12, 283–295. [Google Scholar] [CrossRef] [Green Version]
- Assaid, N.; Mousson, L.; Moutailler, S.; Arich, S.; Akarid, K.; Monier, M.; Beck, C.; Lecollinet, S.; Failloux, A.-B.; Sarih, M. Evidence of circulation of West Nile virus in Culex pipiens mosquitoes and horses in Morocco. Acta Trop. 2020, 205, 105414. [Google Scholar] [CrossRef] [PubMed]
- Assaid, N.; Arich, S.; Ezzikouri, S.; Benjelloun, S.; Dia, M.; Faye, O.; Akarid, K.; Beck, C.; Lecollinet, S.; Failloux, A.-B.; et al. Serological evidence of West Nile virus infection in human populations and domestic birds in the Northwest of Morocco. Comp. Immunol. Microbiol. Infect. Dis. 2021, 76, 101646. [Google Scholar] [CrossRef] [PubMed]
- Lumley, S.; Horton, D.L.; Hernandez-Triana, L.L.M.; Johnson, N.; Fooks, A.R.; Hewson, R. Rift Valley fever virus: Strategies for maintenance, survival and vertical transmission in mosquitoes. J. Gen. Virol. 2017, 98, 875–887. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Clements, A.C.A.; Pfeiffer, D.U.; Martin, V. Application of knowledge-driven spatial modelling approaches and uncertainty management to a study of Rift Valley fever in Africa. Int. J. Health Geogr. 2006, 5, 57. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mahmoud, A.S.; Di Sabatino, D.; Danzetta, M.L.; Iapaolo, F.; Tolari, F.; Forzan, M.; Mazzei, M.; Dayhum, A.; de Massis, F.; Monaco, F. Rift Valley fever virus: A serological survey in Libyan ruminants. Open Vet. J. 2018, 8, 204–207. [Google Scholar] [CrossRef]
- Kenawy, M.A.; Abdel-Hamid, Y.M.; Beier, J.C. Rift Valley Fever in Egypt and other African countries: Historical review, recent outbreaks and possibility of disease occurrence in Egypt. Acta Trop. 2018, 181, 40–49. [Google Scholar] [CrossRef]
- Humphrey, J.M.; Cleton, N.B.; Reusken, C.B.E.M.; Glesby, M.J.; Koopmans, M.; Abu-Raddad, L.J. Urban Chikungunya in the Middle East and North Africa: A systematic review. PLoS Negl. Trop. Dis. 2017, 11, e0005707. [Google Scholar] [CrossRef] [Green Version]
- Darwish, M.A.; Feinsod, F.M.; Scott, R.M.; Ksiazek, T.G.; Botros, B.A.; Farrag, I.H.; El Said, S. Arboviral causes of non-specific fever and myalgia in a fever hospital patient population in Cairo, Egypt. Trans. R. Soc. Trop. Med. Hyg. 1987, 81, 1001–1003. [Google Scholar] [CrossRef]
- World Health Organization. Dengue and Severe Dengue; WHO: Geneva, Switzerland, 2022. [Google Scholar]
- Humphrey, J.M.; Cleton, N.B.; Reusken, C.B.E.M.; Glesby, M.J.; Koopmans, M.P.G.; Abu-Raddad, L.J. Dengue in the Middle East and North Africa: A Systematic Review. PLoS Negl. Trop. Dis. 2016, 10, e0005194. [Google Scholar] [CrossRef] [Green Version]
- Abozeid, S.; Elsayed, A.K.; Schaffner, F.; Samy, A. Re-emergence of Aedes aegypti in Egypt. Lancet Infect. Dis. 2018, 18, 142–143. [Google Scholar] [CrossRef] [Green Version]
- Torres-Flores, J.M.; Reyes-Sandoval, A.; Salazar, M.I. Dengue Vaccines: An Update. BioDrugs 2022, 36, 325–336. [Google Scholar] [CrossRef]
- World Health Organization. Yellow Fever; WHO: Geneva, Switzerland, 2019. [Google Scholar]
- Gianchecchi, E.; Cianchi, V.; Torelli, A.; Montomoli, E. Yellow Fever: Origin, Epidemiology, Preventive Strategies and Future Prospects. Vaccines 2022, 10, 372. [Google Scholar] [CrossRef] [PubMed]
- Abreu, A.D.J.L.D.; Cavalcante, J.R.; Lagos, L.W.d.A.; Caetano, R.; Braga, J.U. A Systematic Review and a Meta-Analysis of the Yellow Fever Vaccine in the Elderly Population. Vaccines 2022, 10, 711. [Google Scholar] [CrossRef] [PubMed]
- Escadafal, C.; Gaayeb, L.; Riccardo, F.; Pérez-Ramírez, E.; Picard, M.; Dente, M.G.; Fernández-Pinero, J.; Manuguerra, J.-C.; Jiménez-Clavero, M.; Declich, S.; et al. Risk of Zika virus transmission in the Euro-Mediterranean area and the added value of building preparedness to arboviral threats from a One Health perspective. BMC Public Health 2016, 16, 1219. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nyaruaba, R.; Mwaliko, C.; Mwau, M.; Mousa, S.; Wei, H. Arboviruses in the East African Community partner states: A review of medically important mosquito-borne Arboviruses. Pathog. Glob. Health 2019, 113, 209–228. [Google Scholar] [CrossRef]
- Turell, M.J.; Morrill, J.C.; Rossi, C.A.; Gad, A.M.; Cope, S.E.; Clements, T.L.; Arthur, R.R.; Wasieloski, L.P.; Dohm, D.J.; Nash, D.; et al. Isolation of West Nile and Sindbis Viruses from Mosquitoes Collected in the Nile Valley of Egypt During an Outbreak of Rift Valley Fever. J. Med. Èntomol. 2002, 39, 248–250. [Google Scholar] [CrossRef]
- Ayhan, N.; Hachid, A.; Thirion, L.; Benallal, K.E.; Pezzi, L.; Khardine, F.A.; Benbetka, C.; Benbetka, S.; Harrat, Z.; Charrel, R. Detection and Isolation of Sindbis Virus from Field Collected Mosquitoes in Timimoun, Algeria. Viruses 2022, 14, 894. [Google Scholar] [CrossRef]
- Clé, M.; Beck, C.; Salinas, S.; Lecollinet, S.; Gutierrez, S.; van de Perre, P.; Baldet, T.; Foulongne, V.; Simonin, Y. Usutu virus: A new threat? Epidemiol. Infect. 2019, 147, e232. [Google Scholar] [CrossRef] [Green Version]
- Socolovschi, C.; Pages, F.; Ndiath, M.O.; Ratmanov, P.; Raoult, D. Rickettsia Species in African Anopheles Mosquitoes. PLoS ONE 2012, 7, e48254. [Google Scholar] [CrossRef] [Green Version]
- Zhang, J.; Lu, G.; Li, J.; Kelly, P.; Li, M.; Wang, J.; Huang, K.; Qiu, H.; You, J.; Zhang, R.; et al. Molecular Detection of Rickettsia felis and Rickettsia bellii in Mosquitoes. Vector-Borne Zoonotic Dis. 2019, 19, 802–809. [Google Scholar] [CrossRef] [Green Version]
- Dieme, C.; Bechah, Y.; Socolovschi, C.; Audoly, G.; Berenger, J.-M.; Faye, O.; Raoult, D.; Parola, P. Transmission potential of Rickettsia felis infection by Anopheles gambiae mosquitoes. Proc. Natl. Acad. Sci. USA 2015, 112, 8088–8093. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zhang, J.; Lu, G.; Kelly, P.J.; Wang, C. Seasonal and Gender Differences in Presence of Rickettsia felis and Blood meals Provide Additional Evidence of a Vector Role for Mosquitoes. Can. J. Infect. Dis. Med. Microbiol. 2019, 2019, 8543460–8543465. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Thelaus, J.; Andersson, A.; Broman, T.; Bäckman, S.; Granberg, M.; Karlsson, L.; Kuoppa, K.; Larsson, E.; Lundmark, E.; Lundström, J.O.; et al. Francisella tularensis Subspecies holarctica Occurs in Swedish Mosquitoes, Persists Through the Developmental Stages of Laboratory-Infected Mosquitoes and Is Transmissible During Blood Feeding. Microb. Ecol. 2013, 67, 96–107. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bäckman, S.; Näslund, J.; Forsman, M.; Thelaus, J. Transmission of tularemia from a water source by transstadial maintenance in a mosquito vector. Sci. Rep. 2015, 5, 7793. [Google Scholar] [CrossRef] [Green Version]
- Kosik-Bogacka, D.I.; Kużna-Grygiel, W.; Jaborowska, M. Ticks and Mosquitoes as Vectors of Borrelia burgdorferi s. l. in the Forested Areas of Szczecin. Folia Biol. 2007, 55, 143–146. [Google Scholar] [CrossRef]
- Melaun, C.; Zotzmann, S.; Santaella, V.G.; Werblow, A.; Zumkowski-Xylander, H.; Kraiczy, P.; Klimpel, S. Occurrence of Borrelia burgdorferi s.l. in different genera of mosquitoes (Culicidae) in Central Europe. Ticks Tick-Borne Dis. 2016, 7, 256–263. [Google Scholar] [CrossRef]
- Rudolf, I.; Blažejová, H.; Mendel, J.; Straková, P.; Šebesta, O.; Rettich, F.; Čabanová, V.; Miterpáková, M.; Betášová, L.; Peško, J.; et al. Bartonella species in medically important mosquitoes, Central Europe. Parasitol Res. 2020, 119, 2713–2717. [Google Scholar] [CrossRef]
- Tourapi, C.; Tsioutis, C. Circular Policy: A New Approach to Vector and Vector-Borne Diseases’ Management in Line with the Global Vector Control Response (2017–2030). Trop. Med. Infect. Dis. 2022, 7, 125. [Google Scholar] [CrossRef]
- Atyame, C.M.; Labbe, P.; Rousset, F.; Beji, M.; Makoundou, P.; Duron, O.; Dumas, E.; Pasteur, N.; Bouattour, A.; Fort, P.; et al. Stable coexistence of incompatibleWolbachiaalong a narrow contact zone in mosquito field populations. Mol. Ecol. 2015, 24, 508–521. [Google Scholar] [CrossRef]
- Tmimi, F.; Bkhache, M.; Mounaji, K.; Failloux, A.; Sarih, M. First report of the endobacteria Wolbachia in natural populations of Culex pipiens in Morocco. J. Vector Ecol. 2017, 42, 349–351. [Google Scholar] [CrossRef] [Green Version]
- Alout, H.; Labbé, P.; Pasteur, N.; Weill, M. High incidence of ace-1 duplicated haplotypes in resistant Culex pipiens mosquitoes from Algeria. Insect Biochem. Mol. Biol. 2011, 41, 29–35. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lalami, A.E.O.; El-Akhal, F.; El Amri, N.; Maniar, S.; Faraj, C. State resistance of the mosquito Culex pipiens towards temephos central Morocco. Bull. Soc. Pathol. Exot. 2014, 107, 194–198. [Google Scholar] [CrossRef]
- Bkhache, M.; Tmimi, F.-Z.; Charafeddine, O.; Faraj, C.; Failloux, A.-B.; Sarih, M. First report of L1014F-kdr mutation in Culex pipiens complex from Morocco. Parasites Vectors 2016, 9, 644. [Google Scholar] [CrossRef] [Green Version]
- Tabbabi, A.; Daaboub, J.; Laamari, A.; Ben Cheikh, R.; Feriani, M.; Boubaker, C.; Ben Jha, I.; Ben Cheikh, H. Evaluation of resistance to temephos insecticide in Culex pipiens pipiens larvae collected from three districts of Tunisia. Afr. Health Sci. 2019, 19, 1361–1367. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tabbabi, A.; Daaboub, J. First studies showing high temephos resistance in Anopheles labranchiae (Diptera: Culicidae) from Tunisia. Afr. Health Sci. 2018, 18, 41–47. [Google Scholar] [CrossRef] [PubMed]
- Tabbabi, A.; Daaboub, J.; Ben Cheikh, R.; Laamari, A.; Feriani, M.; Boubaker, C.; Ben Jha, I.; Ben Cheikh, H. The potential role of urbanization in the resistance to organophosphate insecticide in Culex pipiens pipiens from Tunisia. Afr. Health Sci. 2019, 19, 1368–1375. [Google Scholar] [CrossRef] [Green Version]
- Tabbabi, A.; Daaboub, J.; Ben Cheikh, R.; Laamari, A.; Feriani, M.; Boubaker, C.; Ben Jha, I.; Ben Cheikh, H. Resistance status to deltamethrin pyrethroid of Culex pipiens pipiens (Diptera: Culicidae) collected from three districts of Tunisia. Afr. Health Sci. 2018, 18, 1182–1188. [Google Scholar] [CrossRef]
- Arich, S.; Assaid, N.; Taki, H.; Weill, M.; Labbé, P.; Sarih, M. Distribution of insecticide resistance and molecular mechanisms involved in the West Nile vector Culex pipiens in Morocco. Pest Manag. Sci. 2020, 77, 1178–1186. [Google Scholar] [CrossRef]
- Promed. 2021. Available online: https://promedmail.org/ (accessed on 1 September 2022).
- Bohers, C.; Mousson, L.; Madec, Y.; Vazeille, M.; Rhim, A.; M’Ghirbi, Y.; Bouattour, A.; Failloux, A.-B. The recently introduced Aedes albopictus in Tunisia has the potential to transmit chikungunya, dengue and Zika viruses. PLoS Negl. Trop. Dis. 2020, 14, e0008475. [Google Scholar] [CrossRef]
- Ibáñez-Justicia, A.; Smitz, N.; Hartog, W.D.; van de Vossenberg, B.; de Wolf, K.; Deblauwe, I.; van Bortel, W.; Jacobs, F.; Vaux, A.G.C.; Medlock, J.M.; et al. Detection of Exotic Mosquito Species (Diptera: Culicidae) at International Airports in Europe. Int. J. Environ. Res. Public Health 2020, 17, 3450. [Google Scholar] [CrossRef]
- Ducheyne, E.; Minh, N.N.T.; Haddad, N.; Bryssinckx, W.; Buliva, E.; Simard, F.; Malik, M.R.; Charlier, J.; de Waele, V.; Mahmoud, O.; et al. Current and future distribution of Aedes aegypti and Aedes albopictus (Diptera: Culicidae) in WHO Eastern Mediterranean Region. Int. J. Health Geogr. 2018, 17, 4. [Google Scholar] [CrossRef] [PubMed]
| Species | Diseases | Genome Size (Mb) | G + C (%) | Protein Coding Genes | GenBank Genome ID | Geographic Distribution | Reference |
|---|---|---|---|---|---|---|---|
| Anopheles arabiensis | Malaria | 256.8 | 44.8 | 25,532 | 11,544 | Egypt. | [41] |
| Anopheles coluzzi | Malaria | 273.4 | 44.5 | 23,396 | 41,035 | Algeria, Morocco, Tunisia. | [41] |
| Anopheles stephensi | Malaria | 221 | 44.8 | 11,789 | 2653 | Egypt. | [42] |
| Aedes albopictus | Arboviruses Filariasis | 1967 | 40.4 | 17,539 | 45 | Algeria, Morocco, Tunisia. | [43] |
| Aedes aegypti | Arboviruses | 1376 | 38.2 | 15,419 | 44 | Algeria, Morocco, Egypt, Libya, Tunisia. | [44] |
| Culex quinquefasciatus | Arboviruses Lymphatic filariasis | 579 | 37.4 | 18,883 | 393 | Algeria, Morocco. | [45] |
| Subfamily | Genus | Subgenus | Species | Diseases Transmitted | Distribution | References | ||
|---|---|---|---|---|---|---|---|---|
| Viruses | Parasites | Bacteria | ||||||
| Culicinae | Aedes | Stegomyia | Ae. albopictus | Dengue, Yellow fever **, Chikungunya **, Zika | Filariasis | Rickettsia felis | Algeria Morocco | [54,55] |
| Ae. aegypti | Dengue, Yellow fever **, Chikungunya **, Zika, | Filariasis | / | Algeria, Egypt, Libya, Morocco, Tunisia. | [56] | |||
| Ochlerotatus | Ae. caspius | Rift Valley Fever, West Nile Virus, Usutu Virus | Filariasis | / | Algeria, Egypt, Libya, Morocco, Tunisia. | [57,58] | ||
| Ae. detritus | Rift Valley Fever, WNV | / | / | Algeria, Egypt, Tunisia | [57,58] | |||
| Aedimorphus | Ae. vexans | Rift Valley Fever, | Filariasis | / | Algeria, Morocco | [59,60] | ||
| Culex | Culex | Cx. pipiens | West Nile Virus, Rift Valley Fever Virus, Usutu Virus, | Dirofilaria immitis, D. repens, Wuchereria bancrofti | / | Algeria, Egypt, Libya, Morocco, Tunisia | [57,58,59] | |
| Cx. antennatus | West Nile Virus, Rift Valley Fever Virus | Dirofilaria repens | / | Algeria, Egypt, Tunisia | [61,58] | |||
| Cx. perexiguus | Rift Valley Fever Virus, West Nile Virus, Sindbis virus | / | / | Algeria, Egypt, Libya, Morocco, Tunisia. | [57,58] | |||
| Cx. theileri | Rift Valley Fever Virus, West Nile Virus, Sindbis virus | / | / | Algeria, Egypt, Libya, Morocco, Tunisia. | [57,58] | |||
| Cx. univittatus | West Nile Virus, Sindbis virus | / | / | Egypt | [58] | |||
| Cx. quinquefasciatus | West Nile Virus, Saint Louis encephalitis ** | Wuchereria bancrofti | / | Algeria, Morocco. | [59,62] 1 | |||
| Barraudius | Cx. modestus | WNV, Usutu virus, Tahyna virus **, Lednice virus ** | / | / | Algeria, Morocco | [63] | ||
| Cx. pusillus | / | Dirofilaria immitis | / | Algeria, Egypt, Libya, Tunisia. | [61] | |||
| Culiseta | Culiseta | Cs. annulata | Tahyna virus ** | / | / | Algeria, Morocco, Tunisia. | [21] | |
| Anophelinae | Anopheles | Anopheles | An. labranchiae | / | Plasmodium | / | Algeria, Libya Morocco, Tunisia. | [64] |
| An. algeriensis | / | Plasmodium | / | Algeria, Egypt, Libya, Morocco, Tunisia. | [64,58] | |||
| An. coustani | Rift Valley Fever Virus, Zika | Plasmodium | / | Egypt | [58] | |||
| An. claviger | / | Plasmodium | / | Algeria, Libya, Morocco, Tunisia. | [18,65,66,67] | |||
| An. sachorovi | / | Plasmodium | / | Algeria | [68] | |||
| Cellia | An. multicolor | / | Plasmodium | / | Algeria, Egypt, Libya, Morocco, Tunisia. | [64,58] | ||
| An. coluzzi | O’nyong-nyong ** Tataguine virus **, Nyando virus ** | Plasmodium | Rickettsia felis | Algeria *, Egypt # | [69,70] | |||
| An. sergentii | / | Plasmodium | / | Algeria, Egypt, Libya, Morocco, Tunisia. | [64,58] | |||
| An. superpictus | / | Plasmodium | / | Algeria, Egypt | [17,58] | |||
| An. pharoensis | / | Plasmodium Filariasis | / | Egypt | [58] | |||
| An. stephensi | / | Plasmodium | / | Egypt | [58] | |||
| An. arabiensis | / | Plasmodium | / | Egypt | [18] | |||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nebbak, A.; Almeras, L.; Parola, P.; Bitam, I. Mosquito Vectors (Diptera: Culicidae) and Mosquito-Borne Diseases in North Africa. Insects 2022, 13, 962. https://doi.org/10.3390/insects13100962
Nebbak A, Almeras L, Parola P, Bitam I. Mosquito Vectors (Diptera: Culicidae) and Mosquito-Borne Diseases in North Africa. Insects. 2022; 13(10):962. https://doi.org/10.3390/insects13100962
Chicago/Turabian StyleNebbak, Amira, Lionel Almeras, Philippe Parola, and Idir Bitam. 2022. "Mosquito Vectors (Diptera: Culicidae) and Mosquito-Borne Diseases in North Africa" Insects 13, no. 10: 962. https://doi.org/10.3390/insects13100962