Current Assistive Devices Usage and Recommendations for a Future Artificial Vision Prosthesis among Patients with Severe Visual Impairment Due to Inherited Retinal Diseases
Abstract
:1. Introduction
2. Materials and Methods
3. Results
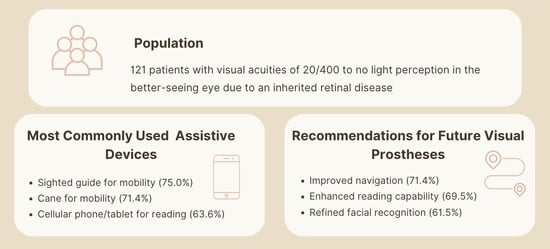
3.1. Activities of Daily Living to Be Improved and Assistive Devices Currently Used
3.2. Recommendations for Designing a Future Artificial Vision Prosthetic Device
3.3. Suggested Improvements for Argus II Prosthesis among Argus Recipients
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Hanany, M.; Rivolta, C.; Sharon, D. Worldwide carrier frequency and genetic prevalence of autosomal recessive inherited retinal diseases. Proc. Natl. Acad. Sci. USA 2020, 117, 2710–2716. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Available online: https://www.who.int/news-room/fact-sheets/detail/blindness-and-visual-impairment (accessed on 20 May 2022).
- Petoe, M.A.; Titchener, S.A.; Kolic, M.; Kentler, W.G.; Abbott, C.J.; Nayagam, D.A. A Second-Generation (44-Channel) Suprachoroidal Retinal Prosthesis: Interim Clinical Trial Results. Transl. Vis. Sci. Technol. 2021, 10, 12. [Google Scholar] [CrossRef] [PubMed]
- Lam, B.L.; Gregori, N.Z. Successes and Challenges of Retinal Implants for Profound Visual Loss from Outer Retinal Degeneration. JAMA Ophthalmol. 2019, 137, 903–904. [Google Scholar] [CrossRef] [PubMed]
- Rizzo, S.; Belting, C.; Cinelli, L.; Allegrini, L.; Genovesi-Ebert, F.; Barca, F.; Di Bartolo, E. The Argus II Retinal Prosthesis: 12-month outcomes from a single-study center. Am. J. Ophthalmol. 2014, 157, 1282–1290. [Google Scholar] [CrossRef] [PubMed]
- Da Cruz, L.; Dorn, J.D.; Humayun, M.S.; Dagnelie, G.; Handa, J.; Barale, P.O. Five-Year Safety and Performance Results from the Argus II Retinal Prosthesis System Clinical Trial. Ophthalmology 2016, 123, 2248–2254. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dagnelie, G.; Christopher, P.; Arditi, A.; da Cruz, L.; Duncan, J.L.; Ho, A.C. Performance of real-world functional vision tasks by blind subjects improves after implantation with the Argus(R) II retinal prosthesis system. Clin. Exp. Ophthalmol. 2017, 45, 152–159. [Google Scholar] [CrossRef] [PubMed]
- Geruschat, D.R.; Richards, T.P.; Arditi, A.; da Cruz, L.; Dagnelie, G.; Dorn, J.D. An analysis of observer-rated functional vision in patients implanted with the Argus II Retinal Prosthesis System at three years. Clin. Exp. Optom. 2016, 99, 227–232. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Simunovic, M.P.; Shen, W.; Lin, J.Y.; Protti, D.A.; Lisowski, L.; Gillies, M.C. Optogenetic approaches to vision restoration. Exp. Eye Res. 2019, 178, 15–26. [Google Scholar] [CrossRef] [PubMed]
- Pio-Lopez, L.; Poulkouras, R.; Depannemaecker, D. Visual cortical prosthesis: An electrical perspective. J. Med. Eng. Technol. 2021, 45, 394–407. [Google Scholar] [CrossRef] [PubMed]
- Prem Senthil, M.; Khadka, J.; Gilhotra, J.S.; Simon, S.; Pesudovs, K. Exploring the quality-of-life issues in people with retinal diseases: A qualitative study. J. Patient Rep. Outcomes 2017, 1, 15. [Google Scholar] [CrossRef] [PubMed]
- Prem Senthil, M.; Khadka, J.; Pesudovs, K. Assessment of patient-reported outcomes in retinal diseases: A systematic review. Surv. Ophthalmol. 2017, 62, 546–582. [Google Scholar] [CrossRef] [PubMed]
- De Koo, L.C.O.; Gregori, N.Z. The Argus II Retinal Prosthesis: A Comprehensive Review. Int. Ophthalmol. Clin. 2016, 56, 39–46. [Google Scholar] [CrossRef] [PubMed]
| Variable | All Respondents | |
|---|---|---|
| n | % | |
| Visual Acuity (n = 121) | ||
| 20/400 | 23 | 19.0% |
| Counting Fingers (CF) | 14 | 11.6% |
| Hand Motion (HM) | 26 | 21.5% |
| Light Perception (LP) | 41 | 33.9% |
| No Light Perception (NLP) | 12 | 9.9% |
| Argus Recipient | 5 | 4.1% |
| Length of Visual Impairment (n = 121) | ||
| Less than 1 year | 9 | 7.4% |
| 1–10 years | 53 | 43.8% |
| More than 10 years | 59 | 48.8% |
| Gender (n = 117) | ||
| Male | 70 | 59.8% |
| Female | 47 | 40.2% |
| Age (n = 116) | ||
| 18–34 years | 15 | 12.9% |
| 35–64 years | 62 | 53.4% |
| 65–80 years | 37 | 31.9% |
| Over 80 years | 2 | 1.7% |
| Race/Ethnicity (n = 118) | ||
| White | 88 | 74.6% |
| Black or African American | 5 | 4.2% |
| Latino, Hispanic, or Spanish origin | 15 | 12.7% |
| Asian | 6 | 5.1% |
| American Indian or Alaska Native | 1 | 0.8% |
| Middle Eastern | 2 | 1.7% |
| Other | 1 | 0.8% |
| Highest Education Completed (n = 114) | ||
| Some High School | 9 | 7.9% |
| High School Graduate | 24 | 21.1% |
| Associate Degree (or some college) | 25 | 21.9% |
| Bachelor’s Degree | 31 | 27.2% |
| Master’s Degree | 18 | 15.8% |
| Doctorate/PhD or higher | 4 | 3.5% |
| Trade School | 3 | 2.6% |
| Primary Country of Residence (n = 116) | ||
| United States of America | 114 | 98.3% |
| Canada | 1 | 0.9% |
| European Country | 1 | 0.9% |
| Geographic Area of Residence (n = 115) | ||
| Rural | 30 | 26.1% |
| Suburban | 58 | 50.4% |
| Urban | 27 | 23.5% |
| Current Vision (n = 114) | ||
| Loss of central vision only | 16 | 14.0% |
| Loss of central and side vision | 98 | 86.0% |
| Inherited Retinal Disease (IRD) (n = 105) | ||
| Retinitis Pigmentosa | 54 | 51.4% |
| Cone-Rod Dystrophy | 10 | 9.5% |
| Stargardt Disease | 10 | 9.5% |
| Choroideremia | 10 | 9.5% |
| Leber Congenital Amaurosis | 4 | 3.8% |
| Other | 12 | 11.4% |
| Multiple diseases | 5 | 4.8% |
| Assistance with Daily Activities (n = 116) | ||
| Has a person who regularly helps | 57 | 49.1% |
| Has a person who occasionally helps | 44 | 37.9% |
| Does not have anyone who helps | 15 | 12.9% |
| Employment Status (n = 109) | ||
| Employed | 27 | 24.8% |
| Unemployed | 82 | 75.2% |
| Volunteering Status (n = 110) | ||
| Volunteer | 20 | 18.2% |
| Non-volunteer | 90 | 81.8% |
| Variable | All Respondents | |
|---|---|---|
| n | % | |
| Activities INSIDE OR OUTSIDE OF HOME due to poor vision without any assistive devices that respondents report as most important to improve or regain (n = 103) | ||
| Reading | 56 | 54.4% |
| Navigating/Exercising/Traveling | 53 | 51.5% |
| Cooking | 41 | 39.8% |
| Using computer or phone/Watching TV | 37 | 35.9% |
| Household Chores/Repairs/Cleaning | 37 | 35.9% |
| Yard work | 24 | 23.3% |
| Hobbies (e.g., doing crafts, playing video games) | 23 | 22.3% |
| Driving | 20 | 19.4% |
| Shop** | 20 | 19.4% |
| Selecting and matching clothing | 13 | 12.6% |
| Locating/identifying objects and people | 12 | 11.7% |
| Recognizing faces and facial expressions | 11 | 10.7% |
| Laundry | 10 | 9.7% |
| Other (managing finances, medical care, professional and academic pursuits, etc.) | 53 | 51.5% |
| Assistive Devices Used for Reading (n = 110) | ||
| Cellular phone/tablet apps and accessibility features | 70 | 63.6% |
| Computer screen reader | 63 | 57.3% |
| Another person | 60 | 54.5% |
| Scanner or hand-held reader | 39 | 35.5% |
| CCTV magnifiers | 29 | 26.4% |
| Magnifying glass | 22 | 20.0% |
| Braille | 20 | 18.2% |
| Other (OrCAM device, computer with large font, digital talking book player, wearable magnifier, electronic magnifier) | 18 | 16.4% |
| None | 3 | 2.7% |
| Assistive Devices Used for Mobility and Orientation (n = 112) | ||
| Another person to assist | 84 | 75.0% |
| Cane | 80 | 71.4% |
| Technological device * | 37 | 33.0% |
| Guide dog | 17 | 15.2% |
| Aira service | 9 | 8.0% |
| None | 5 | 4.5% |
| Argus II retinal prosthesis | 2 | 1.8% |
| Variable | All Respondents | |
|---|---|---|
| n | % | |
| If you could design a bionic eye or prosthetic device to help you OUTDOORS, which activities would be more significant to you (respondents chose 5 statements from the list of 10 choices)? (n = 105) | ||
| It would help avoid bum** into things when walking | 75 | 71.4% |
| It would help me read labels at the grocery store or packages | 73 | 69.5% |
| It would help me identify objects close by | 68 | 64.8% |
| It would help me judge how far objects are away from me | 63 | 60.0% |
| It would help me read street signs and store names | 62 | 59.0% |
| It would help me detect moving objects such as cars | 62 | 59.0% |
| It would help me cross street at a traffic light | 60 | 57.1% |
| It would help me identify objects far away | 56 | 53.3% |
| It would help me walk straight in an open space | 45 | 42.9% |
| It would give me more side vision (wider field of vision) | 36 | 34.3% |
| If you could design a bionic eye or prosthetic device to help you INSIDE, which activities would be more significant to you (respondents chose 5 statements from the list of 18 choices)? (n = 104) | ||
| It would help me recognize faces | 64 | 61.5% |
| It would help me see small objects more clearly | 56 | 53.8% |
| It would help me use a computer without a screen reader | 50 | 48.1% |
| It would help me watch TV or movies | 50 | 48.1% |
| It would help me with household tasks such as cleaning, laundry | 48 | 46.2% |
| It would help me prepare meals or fix a snack | 45 | 43.3% |
| It would help me read single letters and numbers | 44 | 42.3% |
| It would help me sign my name | 39 | 37.5% |
| It would help me identify money | 39 | 37.5% |
| It would help me judge how far objects are away from me | 37 | 35.6% |
| It would help me locate doors | 37 | 35.6% |
| It would help me see colors when matching clothes for example | 36 | 34.6% |
| It would help me locate and track silent people | 30 | 28.8% |
| It would give me more side vision (wider field of vision) | 24 | 23.1% |
| It would help me find clear glass doors | 21 | 20.2% |
| It would help me with hand-eye coordination | 20 | 19.2% |
| It would help me play video games | 12 | 11.5% |
| It would help me identify sizes of objects | 11 | 10.6% |
| If artificial vision could only restore one function of normal vision, please rank the five abilities below from 1 through 5, with “5” being “I definitely want restored”, and “1” being “I don’t need this restored” (n = 101) | Median (Range) | |
| Navigate independently in unfamiliar areas | 3.6 (1–5) | |
| Read normal text, in print and on devices | 3.3 (1–5) | |
| Able to see and recognize individual faces in detail | 3.2 (1–5) | |
| Watch TV or movies and use a computer without a screen reader | 3.0 (1–5) | |
| See colors and patterns in clothing, nature, and art | 2.4 (1–5) | |
| “In order to agree to surgery for artificial vision, I would have to have confidence that the surgery can at least allow me to see…” | ||
| (respondents chose 1 statement from the list of 7 choices) (n = 101) | ||
| Enough facial detail to identify a person | 44 | 43.6% |
| Enough to avoid an obstacle while walking | 39 | 38.6% |
| Enough to know that a person is present, even if I cannot identify them | 8 | 7.9% |
| Enough to locate a cup or utensil on a table | 6 | 5.9% |
| Enough to tell if a sock is black or white | 3 | 3.0% |
| Enough to know if a light is on or off | 1 | 1.0% |
| Enough to find a door | 0 | 0.0% |
| On a scale from 1 to 5, how important is the ability for you to see color as opposed to black and white with artificial vision. (“5” is “Very important”, and “1” is “Not very important”) (n = 103) | Mean (Range) 3.5 (1–5) | |
| Would you agree to have shape-based vision? (n = 101) | ||
| No | 78 | 77.2% |
| Yes | 23 | 22.8% |
| Artificial vision may be limited in how much you can see at one time, it may appear as if you are looking through a straw, and this may require scanning around with your head (pointing your head in different directions) or scanning with your eyes (moving eyes back and forth) to see. Knowing this limitation, would you agree to have the artificial vision procedure? (n = 99) | ||
| No | 28 | 28.3% |
| Yes, I am ok with scanning with my head | 35 | 35.3% |
| Yes, I prefer scanning with my eyes | 36 | 36.4% |
| Variable | All Respondents | |
|---|---|---|
| n | % | |
| If you have had an Argus II implant and are familiar with the artificial vision it provides, what one improvement would you suggest that is most significant to you? (n = 5) | ||
| Add technology able to recognize objects and tell me what they are | 2 | 40.0% |
| Increase ability to avoid objects and obstacles | 1 | 20.0% |
| Improve inversion of image from black-to-white and white-to-black | 1 | 20.0% |
| Make glasses more comfortable | 1 | 20.0% |
| If you have had an Argus II implant and are familiar with the artificial vision it provides, what additional three improvements would you suggest? (n = 3) | ||
| Cut out the busy flashing background | 2 | 66.7% |
| Increase ability to detect movement | 2 | 66.7% |
| Make the field of artificial vision wider | 1 | 33.3% |
| Add technology able to recognize objects and tell me what they are | 1 | 33.3% |
| Improve detection of distances | 1 | 33.3% |
| Increase ability to avoid objects and obstacles | 1 | 33.3% |
| Increase definition of the object’s shapes | 1 | 33.3% |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sidhu, S.; Persad, P.J.; Lam, B.L.; Zann, K.L.; Gregori, N.Z. Current Assistive Devices Usage and Recommendations for a Future Artificial Vision Prosthesis among Patients with Severe Visual Impairment Due to Inherited Retinal Diseases. J. Clin. Med. 2023, 12, 5283. https://doi.org/10.3390/jcm12165283
Sidhu S, Persad PJ, Lam BL, Zann KL, Gregori NZ. Current Assistive Devices Usage and Recommendations for a Future Artificial Vision Prosthesis among Patients with Severe Visual Impairment Due to Inherited Retinal Diseases. Journal of Clinical Medicine. 2023; 12(16):5283. https://doi.org/10.3390/jcm12165283
Chicago/Turabian StyleSidhu, Sophia, Patrice J. Persad, Byron L. Lam, Kasey L. Zann, and Ninel Z. Gregori. 2023. "Current Assistive Devices Usage and Recommendations for a Future Artificial Vision Prosthesis among Patients with Severe Visual Impairment Due to Inherited Retinal Diseases" Journal of Clinical Medicine 12, no. 16: 5283. https://doi.org/10.3390/jcm12165283