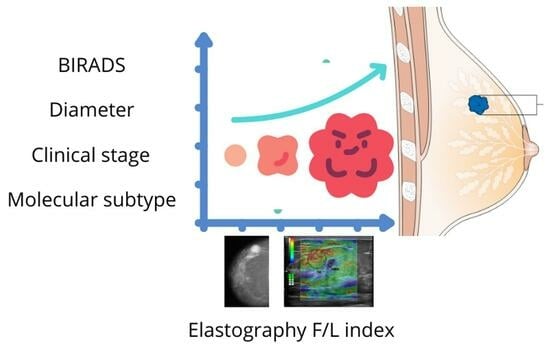
Strain Elastography Fat-to-Lesion Index Is Associated with Mammography BI-RADS Grading, Biopsy, and Molecular Phenotype in Breast Cancer
Abstract
:1. Introduction
| Method | Principle | Invasiveness | Radiation | Detection | Operator-Dependent Bias | Time per Procedure | Cost | Availability | Specificity | Contraindications | References |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Elastography | Through sound waves, tissue stiffness is measured | Minimally invasive | N/A | Useful in suspicious lesions | High variability | Fast procedure | Low cost | Wide availability | Moderate | Patients with conventional ultrasound difficulties | [5] |
| Mammography | Uses X-rays to obtain 2D images of the breast | Breast compression | Ionizing radiation | Useful to identify calcifications | High variability | Fast procedure | Moderate cost | Wide availability | Moderate to low | Not recommended in young or pregnant women | [20] |
| Magnetic resonance imaging (MRI) | Based on the application of magnetic fields and radio waves | Minimally invasive | Non-ionizing radiation | Useful to identify calcifications | Low to moderate variability | Long procedure | High cost | Wide availability but limited use | High | Metallic implants, pacemaker, claustrophobia, kidney disease | [21] |
| Tomosynthesis | Uses X-rays to produce 3D images | Breast compression | Ionizing radiation | Optimized detection in dense tissues | Moderate variability | Fast procedure | Moderate cost | Wide availability | Moderate | Not recommended in young or pregnant women | [22] |
2. Materials and Methods
2.1. Patients
2.2. Ultrasound and Strain Elastography
2.3. Histological and Immunohistochemistry Evaluation
2.4. Clinical Stages in BC
2.5. Statistical Analysis
3. Results
3.1. Principal Component Analysis
3.2. Histological Type, BI-RADS Assignment
3.3. Clinical Stages, Grading Tumors, and Molecular Subtype BC
3.4. Binary Logistic Regression and Neural Network Performance for BC
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization Global Cancer Observatory. Cancer Today. Available online: https://gco.iarc.fr/today/en (accessed on 1 November 2023).
- Iranmakani, S.; Mortezazadeh, T.; Sajadian, F.; Ghaziani, M.F.; Ghafari, A.; Khezerloo, D.; Musa, A.E. A Review of Various Modalities in Breast Imaging: Technical Aspects and Clinical Outcomes. Egypt. J. Radiol. Nucl. Med. 2020, 51, 57. [Google Scholar] [CrossRef]
- Ormachea, J.; Parker, K.J. Elastography Imaging: The 30 Year Perspective. Phys. Med. Biol. 2020, 65, 24TR06. [Google Scholar] [CrossRef] [PubMed]
- Doyley, M.M.; Parker, K.J. Elastography: General Principles and Clincial Applications. Ultrasound Clin. 2014, 9, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Sigrist, R.M.S.; Liau, J.; Kaffas, A.E.; Chammas, M.C.; Willmann, J.K. Ultrasound Elastography: Review of Techniques and Clinical Applications. Theranostics 2017, 7, 1303–1329. [Google Scholar] [CrossRef] [PubMed]
- Chee, C.; Lombardo, P.; Schneider, M.; Danovani, R. Comparison of the Fat-to-Lesion Strain Ratio and the Gland-to-Lesion Strain Ratio With Controlled Precompression in Characterizing Indeterminate and Suspicious Breast Lesions on Ultrasound Imaging. J. Ultrasound Med. 2019, 38, 3257–3266. [Google Scholar] [CrossRef]
- Zhi, H.; **ao, X.-Y.; Yang, H.-Y.; Wen, Y.-L.; Ou, B.; Luo, B.-M.; Liang, B. Semi-Quantitating Stiffness of Breast Solid Lesions in Ultrasonic Elastography. Acad. Radiol. 2008, 15, 1347–1353. [Google Scholar] [CrossRef]
- Franco Uliaque, C.; Pardo Berdún, F.J.; Laborda Herrero, R.; Pérez Lórenz, C. Utilidad de la elastografía semicuantitativa para predecir la malignidad de los nódulos tiroideos. Radiología 2016, 58, 366–372. [Google Scholar] [CrossRef]
- Barr, R.G. Future of Breast Elastography. Ultrasonography 2019, 38, 93–105. [Google Scholar] [CrossRef]
- Youk, J.H.; Son, E.J.; Gweon, H.M.; Han, K.H.; Kim, J.-A. Quantitative Lesion-to-Fat Elasticity Ratio Measured by Shear-Wave Elastography for Breast Mass: Which Area Should Be Selected as the Fat Reference? PLoS ONE 2015, 10, e0138074. [Google Scholar] [CrossRef]
- Seo, M.; Ahn, H.S.; Park, S.H.; Lee, J.B.; Choi, B.I.; Sohn, Y.; Shin, S.Y. Comparison and Combination of Strain and Shear Wave Elastography of Breast Masses for Differentiation of Benign and Malignant Lesions by Quantitative Assessment: Preliminary Study. J. Ultrasound Med. 2018, 37, 99–109. [Google Scholar] [CrossRef]
- Sandrin, L.; Fourquet, B.; Hasquenoph, J.-M.; Yon, S.; Fournier, C.; Mal, F.; Christidis, C.; Ziol, M.; Poulet, B.; Kazemi, F.; et al. Transient Elastography: A New Noninvasive Method for Assessment of Hepatic Fibrosis. Ultrasound Med. Biol. 2003, 29, 1705–1713. [Google Scholar] [CrossRef]
- Fang, C.; Huang, D.Y.; Sidhu, P.S. Elastography of Focal Testicular Lesions: Current Concepts and Utility. Ultrasonography 2019, 38, 302–310. [Google Scholar] [CrossRef]
- Zhao, C.-K.; Xu, H.-X. Ultrasound Elastography of the Thyroid: Principles and Current Status. Ultrasonography 2019, 38, 106–124. [Google Scholar] [CrossRef] [PubMed]
- Yılmaz, E.; Yılmaz, A.; Aslan, A.; Inan, I.; Evren, M.C.; Tekesin, K. Real-Time Elastography for Differentiation of Breast Lesions. Pol. J. Radiol. 2017, 82, 664–669. [Google Scholar] [CrossRef] [PubMed]
- ElMowalled, S. Value of Ultrasound Elastography in Combined with Mammography in Evaluation of Indeterminate Breast Lesions. Benha J. Appl. Sci. 2023, 8, 126–134. [Google Scholar] [CrossRef]
- D’Orsi, C.; Sickles, E.; Mendelson, E.; Morris, E. ACR BI-RADS® Ultrasound. In ACR BI-RADS® Atlas, Breast Imaging Reporting and Data System, 5th ed.; American College of Radiology: Reston, VA, USA, 2013; Volume 1, pp. 128–130. ISBN 9781559030168. [Google Scholar]
- You, Y.; Song, Y.; Li, S.; Ma, Z.; Bo, H. Quantitative and Qualitative Evaluation of Breast Cancer Prognosis: A Sonographic Elastography Study. Med. Sci. Monit. 2019, 25, 9272–9279. [Google Scholar] [CrossRef] [PubMed]
- Farrokh, A.; Wojcinski, S.; Degenhardt, F. Diagnostische Aussagekraft der Strain-Ratio-Messung zur Unterscheidung zwischen malignen und benignen Brusttumoren. Ultraschall Med. 2010, 32, 400–405. [Google Scholar] [CrossRef] [PubMed]
- Heywang-Köbrunner, S.H.; Hacker, A.; Sedlacek, S. Advantages and Disadvantages of Mammography Screening. Breast Care 2011, 6, 199–207. [Google Scholar] [CrossRef] [PubMed]
- Radhakrishna, S.; Agarwal, S.; Parikh, P.M.; Kaur, K.; Panwar, S.; Sharma, S.; Dey, A.; Saxena, K.K.; Chandra, M.; Sud, S. Role of Magnetic Resonance Imaging in Breast Cancer Management. South Asian J. Cancer 2018, 7, 69–71. [Google Scholar] [CrossRef]
- Kleinknecht, J.H.; Ciurea, A.I.; Ciortea, C.A. Pros and Cons for Breast Cancer Screening with Tomosynthesis—A Review of the literature. Med. Pharm. Rep. 2020, 93, 335–341. [Google Scholar] [CrossRef]
- Barr, R.G.; Nakashima, K.; Amy, D.; Cosgrove, D.; Farrokh, A.; Schafer, F.; Bamber, J.C.; Castera, L.; Choi, B.I.; Chou, Y.-H.; et al. WFUMB Guidelines and Recommendations for Clinical Use of Ultrasound Elastography: Part 2: Breast. Ultrasound Med. Biol. 2015, 41, 1148–1160. [Google Scholar] [CrossRef]
- Niknejad, M.; Weerakkody, Y. Breast Imaging-Reporting and Data System (BI-RADS). Radiopaedia.org. 2010. Available online: https://doi.org/10.53347/rID-10003 (accessed on 3 November 2023).
- Gnant, M.; Harbeck, N.; Thomssen, C. St. Gallen 2011: Summary of the Consensus Discussion. Breast Care 2011, 6, 136–141. [Google Scholar] [CrossRef]
- Thomssen, C.; Balic, M.; Harbeck, N.; Gnant, M. St. Gallen/Vienna 2021: A Brief Summary of the Consensus Discussion on Customizing Therapies for Women with Early Breast Cancer. Breast Care 2021, 16, 135–143. [Google Scholar] [CrossRef]
- Giuliano, A.E.; Edge, S.B.; Hortobagyi, G.N. Eighth Edition of the AJCC Cancer Staging Manual: Breast Cancer. Ann. Surg. Oncol. 2018, 25, 1783–1785. [Google Scholar] [CrossRef]
- Zhu, J.-Y.; He, H.-L.; Jiang, X.-C.; Bao, H.-W.; Chen, F. Multimodal Ultrasound Features of Breast Cancers: Correlation with Molecular Subtypes. BMC Med. Imaging 2023, 23, 57. [Google Scholar] [CrossRef]
- Hayashi, M.; Yamamoto, Y.; Sueta, A.; Tomiguchi, M.; Yamamoto-Ibusuki, M.; Kawasoe, T.; Hamada, A.; Iwase, H. Associations Between Elastography Findings and Clinicopathological Factors in Breast Cancer. Medicine 2015, 94, e2290. [Google Scholar] [CrossRef] [PubMed]
- **, Y.; Fenghua, L.; **g, D.; Yifen, G. Strain Elastography Features in Invasive Breast Cancer: Relationship between Stiffness and Pathological Factors. Int. J. Clin. Exp. Med. 2017, 10, 13290–13297. [Google Scholar]
- Togawa, R.; Pfob, A.; Büsch, C.; Alwafai, Z.; Balleyguier, C.; Clevert, D.; Duda, V.; Fastner, S.; Goncalo, M.; Gomez, C.; et al. Potential of Lesion-to-Fat Elasticity Ratio Measured by Shear Wave Elastography to Reduce Benign Biopsies in BI-RADS 4 Breast Lesions. J. Ultrasound Med. 2023, 42, 1729–1736. [Google Scholar] [CrossRef] [PubMed]
- Patel, B.K.; Pepin, K.; Brandt, K.R.; Mazza, G.L.; Pockaj, B.A.; Chen, J.; Zhou, Y.; Northfelt, D.W.; Anderson, K.; Kling, J.M.; et al. Association of Breast Cancer Risk, Density, and Stiffness: Global Tissue Stiffness on Breast MR Elastography (MRE). Breast Cancer Res. Treat. 2022, 194, 79–89. [Google Scholar] [CrossRef] [PubMed]
- Rodríguez-Rodríguez, J.E.; Ioannidis, A.G.; Medina-Muñoz, S.G.; Barberena-Jonas, C.; Blanco-Portillo, J.; Quinto-Cortés, C.D.; Moreno-Estrada, A. The Genetic Legacy of the Manila Galleon Trade in Mexico. Philos. Trans. R. Soc. B 2022, 377, 20200419. [Google Scholar] [CrossRef] [PubMed]
- Lee, N.-R.; Oh, H.-K.; Jeong, Y.-J. Clinical Significance of Ultrasound Elastography and Fibrotic Focus and Their Association in Breast Cancer. J. Clin. Med. 2022, 11, 7435. [Google Scholar] [CrossRef] [PubMed]
- Çorapli, M.; Bulut, H.T.; Örmecï, A.G.; Alakuş, H. Relationship between Strain Elastography and Histopathological Parameters in Breast Cancer. Cukurova Med. J. 2022, 47, 1663–1669. [Google Scholar] [CrossRef]
- Shehata, R.M.A.; El-Sharkawy, M.A.M.; Mahmoud, O.M.; Kamel, H.M. Qualitative and Quantitative Strain and Shear Wave Elastography Paradigm in Differentiation of Breast Lesions. Egypt. J. Radiol. Nucl. Med. 2022, 53, 23. [Google Scholar] [CrossRef]
- Mutala, T.M.; Mwango, G.N.; Aywak, A.; Cioni, D.; Neri, E. Determining the Elastography Strain Ratio Cut off Value for Differentiating Benign from Malignant Breast Lesions: Systematic Review and Meta-Analysis. Cancer Imaging 2022, 22, 12. [Google Scholar] [CrossRef]







| Descriptives Statistics | Age | Tumor Diameter | F/L Index | |||
|---|---|---|---|---|---|---|
| Biopsy result | Neg | Pos | Neg | Pos | Neg | Pos |
| Median | 49.50 | 50.00 | 14.00 | 24.00 | 2.96 | 11.66 |
| Mean | 50.64 | 51.38 | 16.88 | 24.20 | 3.70 | 18.10 |
| SD | 10.81 | 10.80 | 12.86 | 17.67 | 2.57 | 17.01 |
| p-value of Shapiro-Wilk | 0.18 | 0.61 | <0.001 * | <0.001 * | <0.001 * | <0.001 * |
| Malignant Tumors | n | Percent (%) |
|---|---|---|
| IDC | 94 | 87.04% |
| ILC | 10 | 9.26% |
| Missing | 4 | 3.70% |
| Total | 108 | 100.00% |
| Benign tumors | n | Percent (%) |
| Fibroadenoma | 59 | 54.63% |
| Fibrocystic | 9 | 8.33% |
| Ductal Hyperplasia | 15 | 13.89% |
| Lobular Hyperplasia | 1 | 0.93% |
| Atypia | 2 | 1.85% |
| Other benign changes | 22 | 20.37% |
| Total | 108 | 100.00% |
| BI-RADS | n | Percent (%) |
| 2 | 5 | 2.31% |
| 3 | 29 | 13.43% |
| 4A | 50 | 23.15% |
| 4B | 30 | 13.89% |
| 4C | 32 | 14.81% |
| 5 | 65 | 30.09% |
| 6 | 5 | 2.31% |
| Total | 216 | 100.00% |
| Stage | n | Percent (%) |
|---|---|---|
| I | 16 | 14.81% |
| II | 37 | 34.26% |
| III | 42 | 38.89% |
| IV | 10 | 9.26% |
| Not reported | 3 | 2.78% |
| Total | 108 | 100.00% |
| Grade | n | Percent (%) |
| 1 | 2 | 1.85% |
| 2 | 76 | 70.37% |
| 3 | 21 | 19.44% |
| Not reported | 9 | 8.33% |
| Total | 108 | 100.00% |
| Molecular subtype | n | Percent (%) |
| HER2-enriched | 12 | 11.11% |
| Luminal A | 36 | 33.33% |
| Luminal B | 38 | 35.19% |
| TN | 17 | 15.74% |
| Not reported | 5 | 4.63% |
| Total | 108 | 100.00% |
| Subtype | n | Mean | Median | SD | SE | Coefficient of Variation |
|---|---|---|---|---|---|---|
| Luminal A | 36 | 19.34 | 13.60 | 16.73 | 2.79 | 0.87 |
| Luminal B | 38 | 16.53 | 11.70 | 15.35 | 2.49 | 0.93 |
| HER2-enriched | 12 | 29.66 | 22.00 | 24.42 | 7.05 | 0.82 |
| TN | 17 | 10.15 | 6.08 | 9.52 | 2.31 | 0.94 |
| Intra-Group Comparison | Uncorrected p-Value | Bonferroni p Value | FDR p-Value |
|---|---|---|---|
| Luminal A—Luminal B | 0.38 | 1.00 | 0.48 |
| Luminal A—HER2-enriched | 0.48 | 1.00 | 0.48 |
| Luminal A—TN | 0.007 | 0.048 * | 0.024 * |
| Luminal B—HER2-enriched | 0.18 | 1.00 | 0.36 |
| Luminal B—TN | 0.05 | 0.288 | 0.48 |
| HER2-enriched–TN | 0.006 | 0.041 * | 0.024 * |
| Wald Test | 95% CI | ||||
|---|---|---|---|---|---|
| Standard Error | Odds Ratio | p | Lower Bound | Upper Bound | |
| Age | 0.01 | 0.95 | <0.001 | −0.07 | −0.04 |
| F/L index | 0.06 | 1.48 | <0.001 | 0.27 | 0.52 |
| Tumor diameter | 0.01 | 1.01 | 0.62 | −0.02 | 0.03 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cruz-Ramos, J.A.; Trapero-Corona, M.I.; Valencia-Hernández, I.A.; Gómez-Vargas, L.A.; Toranzo-Delgado, M.T.; Cano-Magaña, K.R.; De la Mora-Jiménez, E.; del Carmen López-Armas, G. Strain Elastography Fat-to-Lesion Index Is Associated with Mammography BI-RADS Grading, Biopsy, and Molecular Phenotype in Breast Cancer. Biosensors 2024, 14, 94. https://doi.org/10.3390/bios14020094
Cruz-Ramos JA, Trapero-Corona MI, Valencia-Hernández IA, Gómez-Vargas LA, Toranzo-Delgado MT, Cano-Magaña KR, De la Mora-Jiménez E, del Carmen López-Armas G. Strain Elastography Fat-to-Lesion Index Is Associated with Mammography BI-RADS Grading, Biopsy, and Molecular Phenotype in Breast Cancer. Biosensors. 2024; 14(2):94. https://doi.org/10.3390/bios14020094
Chicago/Turabian StyleCruz-Ramos, José Alfonso, Mijaíl Irak Trapero-Corona, Ingrid Aurora Valencia-Hernández, Luz Amparo Gómez-Vargas, María Teresa Toranzo-Delgado, Karla Raquel Cano-Magaña, Emmanuel De la Mora-Jiménez, and Gabriela del Carmen López-Armas. 2024. "Strain Elastography Fat-to-Lesion Index Is Associated with Mammography BI-RADS Grading, Biopsy, and Molecular Phenotype in Breast Cancer" Biosensors 14, no. 2: 94. https://doi.org/10.3390/bios14020094